Scroll to:
Dynamics of age characteristics and prevalence of concomitant cardiovascular and non-sardiovascular diseases in patients hospitalized with COVID-19 during epidemic wave: data from TARGET-VIP registry
https://doi.org/10.15829/1728-8800-2021-3106
Abstract
Aim. According to hospital-based registry, to evaluate the age characteristics and prevalence of concomitant cardiovascular and non-сardiovascular diseases in patients hospitalized with COVID-19 during epidemic wave.
Material and methods. The TARGET-VIP register included 1130 patients aged 57,5+12,8 years (men, 51,2%) hospitalized at the Pirogov National Medical and Surgical Center from April 6, 2020 to June 22, 2020 with COVID-19. Cardiovascular diseases (CVDs) were diagnosed in 51,6% of patients, non-сardiovascular chronic diseases — in 48,6%, while CVDs and/or non-сardiovascular chronic diseases — in 65,8% of patients.
Results. The average age of patients significantly increased by an average of 0,77 years per week (p<0,001), while the difference between the 1st week (52,8 years) and 11th week (62,2 years) was 9,4 years; the proportion of men did not change significantly. The proportion of patients with CVDs increased significantly — from 34,2% to 66,7%, on average by 3,7% per week (p<0,001; Incidence Risk Ratio (IRR)=1,037; 95% confidence interval (CI), 1,017-1,058), with chronic non-cardiovascular diseases — from 32,5% to 43,2%, on average by 2,5% per week (p<0,001; IRR=1,025; 95% CI, 1,002-1,049), as well as those with CVDs and/or chronic non-cardiovascular diseases — from 47,5% to 75,3%, on average by 3,2% per week (p<0,001; IRR=1,032; 95% CI, 1,017-1,048). Over the entire period, the proportion of people with hypertension (HTN) was 47,0%, with coronary artery disease (CAD) — 15,4%, with heart failure (HF) — 4,0%, and with atrial fibrillation (AF) — 10,1%. The proportion of patients with HTN increased by 9,5% (p<0,001; OR=1,095; 95% CI, 1,047-1,144), with СAD — by 9,4% (p=0,01; OR=1,094; 95% CI, 1,022-1,172) and with AF — by 9,4% (p<0,001; OR=1,094; 95% CI, 1,023-1,170) per week. The proportion of patients with diabetes was 16,5%, with respiratory diseases — 11,4%, with chronic kidney disease (CKD) — 12,6%, with digestive diseases — 22,5%, with obesity — 6,1%. During the epidemic wave, the most pronounced increase in the proportion of patients with CKD was by 6,2% (p=0,036; OR=1,062; 95% CI, 1,004-1,124) and with digestive diseases — by 6,0% (p=0,01; OR=1,060; 95% CI, 1,014-1,109) per week.
Conclusion. According to the 11-week TARGET-VIP registry, the age of patients increased by 9,4 years, CVD cases — by 1,9 times (mainly HTN, CAD, AF), and chronic nonсardiovascular pathology — by 1,3 times (mainly CKD and digestive diseases). These trends in hospital practice corresponded to a weekly increase in the proportion of patients with a higher risk of fatal and non-fatal complications, which is the basis for further research in order to develop a system for a comprehensive prognostic assessment of the degree and rate of increase in the load on hospitals during COVID-19 epidemic wave.
Keywords
For citations:
Lukyanov M.M., Martsevich S.Yu., Pulin A.A., Kutishenko N.P., Andreenko E.Yu., Voronina V.P., Dindikova V.A., Dmitrieva N.A., Zagrebelny A.V., Makoveeva A.N., Lerman O.V., Okshina E.Yu., Sgibneva А.S., Smirnov A.A., Belova E.N., Klyashtorny V.G., Kudryashov E.V., Karpov O.E., Drapkina O.M. Dynamics of age characteristics and prevalence of concomitant cardiovascular and non-sardiovascular diseases in patients hospitalized with COVID-19 during epidemic wave: data from TARGET-VIP registry. Cardiovascular Therapy and Prevention. 2021;20(8):3106. https://doi.org/10.15829/1728-8800-2021-3106
Introduction
The pandemic of coronavirus disease 2019 (COVID-19) has claimed the lives of more than 5 million people and damaged the economic and social life of the entire world community. Every week, millions of new cases continue to be registered worldwide [1][2]. At the same time, age, concomitant cardiovascular (CVD) and non-cardiovascular diseases have an important prognostic value in COVID-19 patients [3- 10]. However, in this category of patients, the dynamics of age and sex characteristics, the detection rate of concomitant CVD and non-cardiovascular diseases during the epidemic wave of COVID-19, in particular, among hospitalized patients, have been little studied. The TARGET-VIP prospective in-hospital registry created in Russia makes it possible to study the clinical and anamnestic characteristics, structure and dynamics of comorbidity in patients with COVID-19 during the epidemic wave.
Based on the foregoing, the aim of the study was to evaluate the age characteristics and prevalence of concomitant cardiovascular and non-cardiovascular diseases in patients hospitalized with COVID-19 during epidemic wave.
Material and methods
The TARGET-VIP registry includes 1130 patients hospitalized at the Pirogov National Medical and Surgical Center from April 6, 2020 to June 22, 2020 due to COVID-19 (age, 57,5±12,8 years; men, 51,2%). Concomitant CVDs was diagnosed in 51,6% of patients, while chronic non-CVDs — in 48,6%, CVDs and/or nonCVDs — in 65,8%. At 11-week enrollment period, corresponding to the epidemic wave in Moscow, the number of new COVID-19 cases in Moscow on April 6, 2020 and June 22, 2020 was 691 and 662, respectively, and the maximum number (6703 cases) was registered on May 07, 2020. The weekly dynamics of average patient age and the proportion of following CVDs was assessed: hypertension (HTN); coronary artery disease (CAD); heart failure (HF); atrial fibrillation (AF); prior myocardial infarction (MI) and stroke. The dynamics of the proportion of following chronic non-CVDs was also assessed: diabetes, respiratory diseases (RDs), chronic kidney disease (CKD), digestive diseases (DDs), anemia, and obesity.
Descriptive statistics were used for statistical data processing. Numerical data are presented as M±SD or Me [Q25%; Q75%]. The statistical significance of differences in numerical data was assessed using the Student’s test, while categorical data — using the χ2 test. For assessing weekly dynamics, regression analysis was used. For binary variables (sex, presence of certain diseases), logistic regression was used with an odds ratio (OR) and 95% confidence interval (CI). For data on the number of certain diseases (number of CVDs, chronic non-CVDs or their sum), Poisson regression was used with an Incidence Risk Ratio (IRR) and corresponding 95% CI. Sex and age of patients were included as covariates in the regression models. Differences were considered significant at p<0,05. Statistical processing was performed using Statistica 7.0 and Stata 15.0 software.
Results
The dynamics of age, sex characteristics and comorbidities in patients admitted is presented in Table 1. The mean age of patients over 11-week period increased significantly, on average, by 0,77 years per week, while this parameter for the first (52,8 years) and 11th weeks (62,2 years) differed by 9,4 years. The proportion of men did not change significantly during the followup, with a maximum of 56,3% in the first week and a minimum of 48,2% in the 11th week (p=0,145; OR=0,973; 95% CI: 0,938-1,009). From the 1st to the 11th week of the inclusion period, the proportion of people with CVDs increased by 1,9 times, with chronic non-CVDs — by 1,3 times, and with both types of pathology — by 1,6 times.
The proportion of patients with CVDs increased significantly, with the CVD number per patient increasing by an average of 3,7% per week (p<0,001; IRR=1,037; 95% CI: 1,017-1,058). The proportion of patients with CVD was the lowest in the 1st week (34,2%) and the highest during the 8th and 11th weeks (68,9 and 66,7%). The average number of chronic nonCVDs per patient significantly increased by 2,5% per week (p<0,001; IRR=1,025; 95% CI: 1,002-1,049). The proportion of patients with CVD and/or chronic nonCVDs increased from 47,5 to 75,3% during the analyzed period. The mean number of CVDs and/or chronic non-CVDs increased by 3,2% per week (p<0,001; IRR=1,032; 95% CI: 1,017-1,048).
Over the entire period of epidemic wave, the proportion of people with hypertension, on average, was 47,0%, with CAD without MI — 15,4%. At the same time, the proportion of patients with prior MI and stroke averaged 5,0 and 4,0%, while the proportion of patients with CAD and AF was 4,0 and 10,1%, respectively. Dynamics of CVD detection rate in analyzed patients during the study period is presented in Table 2. During the epidemic wave from the 1st to the 11th week, the most pronounced increase was noted in patients HTN (from 30,0 to 64,2%, i.e. 2,1 times; p<0,001), CAD (from 13,2 to 37,3%, i.e. 2,8 times; p<0,001) and AF (from 7,1 to 21,0%, i.e. 3,0 times; p<0,001). The proportion of patients with HTN per week increased on average by 9,5% (p<0,001; OR=1,095; 95% CI: 1,047-1,144), with CAD without MI — by 9,4% (p=0,01; OR=1,094; 95% CI: 1,022-1,172) and with AF by 9,4% (p<0,001; OR=1,094; 95% CI: 1,023-1,170). There was no significant weekly increase in the proportion of patients with CAD who underwent MI and stroke (p>0,05).
During 11-week period, the proportion of patients with diabetes, on average, was 16,5%, with respiratory diseases — 11,4%, with CKD — 12,6%, with DDs — 22,5%, with anemia — 3,5%, and with obesity — 6,1%. The dynamics of the detection rate of chronic non-CVDs is presented in Table 3. Of the analyzed chronic non-CVDs, to the greatest extent for 11-week period the proportion of patients with CKD (from 6,7 to 19,8%, i.e. 3,0 times; p<0,001) and DDs (from 14,6 to 24,7%, i.e. in 1,7 times; p=0,037) increased. During the epidemic wave, the most pronounced increase in the proportion of patients with DDS was noted. The proportion of CKD patients increased by an average of 6,2% per week (p=0,036; OR=1,062; 95% CI: 1,004- 1,124), and those with CKD increased by 6,0% (p=0,01; OR=1,060; 95% CI: 1,014-1,109). There was no significant weekly increase in the proportion of patients with diabetes, RDs, anemia and obesity (p>0,05).
Table 1
Dynamics of age, sex characteristics and noncommunicable diseases in patients admitted to the center for COVID-19 and community-acquired pneumonia during the enrollment period
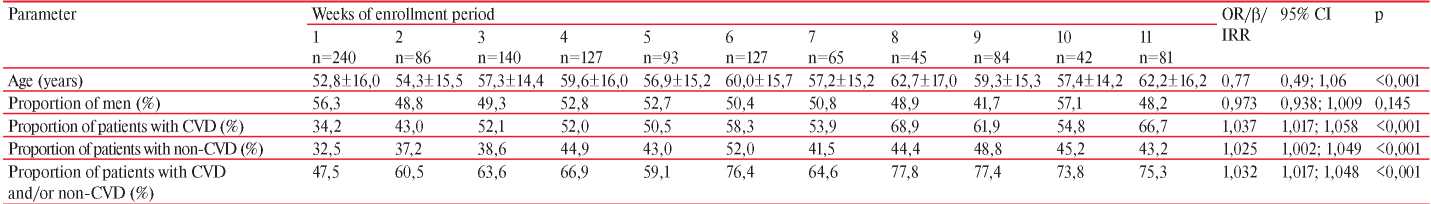
Note: OR (for “proportion of men”), β — «coefficient β» (for “age”), IRR (for “proportion of patients with CVD”, “proportion of patients with non-CVD” and for a combination of these parameters). CI — confidence interval, OR — odds ratio, CVD — cardiovascular diseases.
Table 2
Dynamics of CVD detection rate in patients admitted to the center for COVID-19 and community-acquired pneumonia during the enrollment period
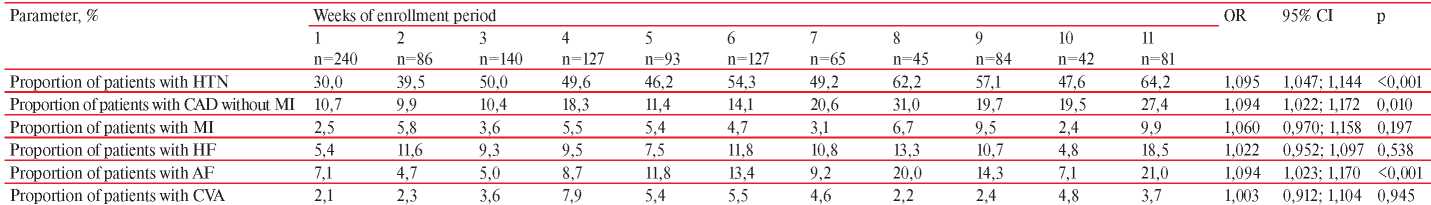
Note: CVA — all cases of MI and transient ischemic attack. MI and CVA is taken into account on the date of hospitalization; MI and CVA developed in the hospital are not taken into account. HTN — hypertension, CI — confidence interval, CAD — coronary artery disease, MI — myocardial infarction, CVA — cerebrovascular accident, OR — odds ratio, AF — atrial fibrillation, HF — heart failure.
Table 3
Dynamics of non-CVD detection rate in patients admitted to the center for COVID-19 and community-acquired pneumonia during the enrollment period
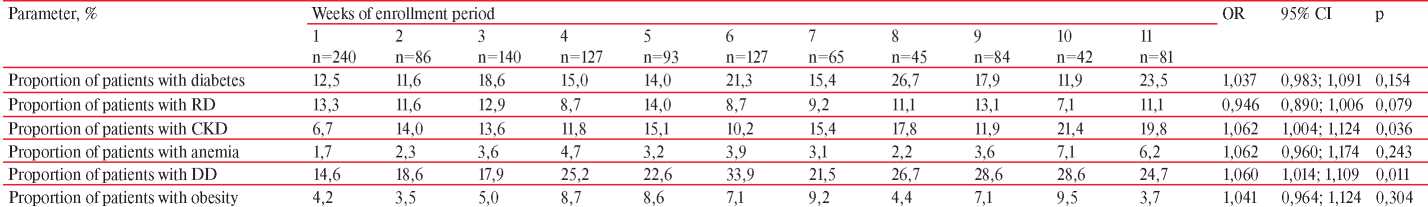
Note: RD — respiratory diseases, DD — digestive diseases, CI — confidence interval, OR — odds ratio, CKD — chronic kidney disease.
Discussion
Monitoring of COVID-19 patients in a pandemic, according to published data, revealed that the severity of its clinical course increases with older patients, and the prognosis in the studied cohorts of patients worsens not only with an increase in the proportion of elderly patients, but also with an increase in the proportion of people with CVD and/or chronic non-CVDs (in particular, with diabetes, respiratory diseases, DDs, cancer, obesity) [6-9][11][12]. In addition, as with other respiratory tract infections, COVID-19 can not only worsen the course of CVD and non-CVDs, but also lead to cardiovascular events [6][13-17].
TARGET-VIP registry revealed a significant weekly increase in the age and detection rate of concomitant CVDs and non-CVDs over 11-week inclusion period, which largely corresponded to the dates of the most pronounced part of COVID-19 wave. Thus, with each subsequent week of the inclusion period during the epidemic wave among hospitalized patients, the risk of fatal and non-fatal complications increased. This is an unfavorable factor, since severe patients are not only more difficult to treat [2][17][18], but they also have a longer length of hospital stay [4][5][7-9]. The above together leads to a progressive increase in the hospital load during the epidemic wave of COVID-19 [2][17][18]. Perhaps one of the reasons for this is that at the beginning of epidemic, predominantly more mobile and young people were infected, from which older members of their families and labor collectives subsequently became infected, significant part of whom had higher prevalence of noncommunicable diseases.
A more detailed analysis of the severity and rates of increase in the risk of fatal and non-fatal complications in patients hospitalized with COVID-19 will, in the future, make it possible to predict an increase in hospital load with each subsequent week of the epidemic wave. It seems very important to compare data over the epidemic wave period on the dynamics of age and detection rate of significant comorbidities in specific hospitals in certain cities and regions as a whole, in particular for Moscow. If a significant correlation is found in a particular hospital and in a corresponding region, there will be an additional opportunity to predict the hospital load in the context of subsequent epidemic waves in order to optimize inpatient care. This is the subject of further research.
Conclusion
According to the 11-week TARGET-VIP registry, the age of patients increased by 9,4 years, CVD cases — by 1,9 times (mainly HTN, CAD, AF), and chronic non-сardiovascular pathology — by 1,3 times (mainly CKD and digestive diseases). These trends in hospital practice corresponded to a weekly increase in the proportion of patients with a higher risk of fatal and non-fatal complications, which is the basis for further research in order to develop a system for a comprehensive prognostic assessment of hospital load during COVID-19 epidemic wave.
Relationships and Activities: none.
References
1. World Health Organization. COVID-19 Weekly Epidemiological Update, 30 November 2021 (https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---30-november-2021).
2. Temporary methodological recommendations. Prevention, diagnosis and treatment of new coronavirus infection (COVID-19). Version 13.1 of 1711.2021. M. 2021. (In Russ.)
3. Drapkina OM, Drozdova LYu, Boitsov SA, et al. Temporary methodological recommendations: “Provision of outpatient medical care to patients with chronic diseases subject to dispensary monitoring in the context of the COVID-19 pandemic”. The Russian Journal of Preventive Medicine. 2020;23(3):2004-41. (In Russ.) doi:10.17116/profmed2020230324.
4. Drapkina OM, Karpov OE, Loukianov MM, et al. Experience of creating and the first results of the prospective hospital registry of patients with suspected or confirmed coronavirus infection (COVID-19) and community-acquired pneumonia (TARGET-VIP). The Russian Journal of Preventive Medicine. 2020;23(8):6-13. (In Russ.) doi:10.17116/profmed2020230816.
5. Drapkina OM, Karpov OE, Loukianov MM, et al. Prospective in-hospital registry of patients with suspected or documented COVID-19 infection and community acquired pneumonia (TARGET-VIP): characteristics of patients and assessment of in-hospital outcomes. Cardiovascular Therapy and Prevention. 2020;19(6):2727 (In Russ.) doi:10.15829/1728880020202727.
6. Konradi AO, Villevalde SV, Duplyakov DV, et al. An openlabel multicenter observational study (registry) of patients recovered from coronavirus disease 2019 (COVID19) with involvement of the cardiovascular system or with baseline severe cardiovascular diseases: rationale, design, and implications for clinical practice. Russian Journal of Cardiology. 2021;26(1):4287. (In Russ.) doi:10.15829/1560407120214287.
7. Arutyunov GP, Tarlovskaya EI, Arutyunov AG, et al. International register “Dynamics analysis of comorbidities in SARSCoV2 survivors” (AKTIV SARSCoV2): analysis of 1,000 patients. Russian Journal of Cardiology. 2020;25(11):4165. (In Russ.) doi:10.15829/1560407120204165.
8. Arutyunov GP, Tarlovskaya EI, Arutyunov AG, et al. International register “Dynamics analysis of comorbidities in SARSCoV2 survivors” (AKTIV SARSCoV2): analysis of predictors of shortterm adverse outcomes in COVID19. Russian Journal of Cardiology. 2021;26(4):4470. (In Russ.) doi:10.15829/1560407120214470.
9. Arutyunov GP, Tarlovskaya EI, Arutyunov AG, et al. International register “Dynamics analysis of comorbidities in SARSCoV2 survivors” (AKTIV) and the register “Analysis of hospitalizations of comorbid patients infected during the second wave of SARSCoV2 outbreak” (AKTIV). Russian Journal of Cardiology. 2021;26(3):4358. (In Russ.) doi:10.15829/1560-4071-2021-4358.
10. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected — obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. 2021;17:135-49. doi: 10.1038/ s41574-020-00462-1.
11. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430-6. doi:10.1038/s41586-020-2521-4.
12. Mehra MR, Desai SS, Kuy SR, et al. Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19. N Engl J Med. 2020;382(26):2582. doi:10.1056/NEJMoa2007621.
13. Wang Y, Wang Z, Tse G, et al. Cardiac arrhythmias in patients with COVID-19. J Arrhythm. 2020;36(5):827-36. doi: 10.1002/joa3.12405.
14. Fun Q, Zhu H, Zhao J, et al. Risk factors for myocardial injury in patients with coronavirus disease 2019 in China. ESC Heart Fail. 2020;10.1002/ehf2.13022. doi:10.1002/ehf2.13022.
15. Shlyakhto EV, Konradi AO, Villevalde SV, et al. Guidelines for the diagnosis and treatment of circulatory diseases in the context of the COVID-19 pandemic. Russian Journal of Cardiology. 2020;25(3):3801. (In Russ.) doi:10.15829/1560-4071-2020-3-3801.
16. Bubnova MG, Shlyakhto EV, Aronov DM, et al. Coronavirus disease 2019: features of comprehensive cardiac and pulmonary rehabilitation. Russian Journal of Cardiology. 2021;26(5):4487. (In Russ.) doi:10.15829/1560-4071-2021-4487
17. 17 Kamalov AA, Mareev VY, Orlova IA. Conceptual approaches to finding effective treatment for a new coronavirus infection at different stages. Annals of the Russian academy of medical sciences. 2021;76(1):43-50. (In Russ.) doi:10.15690/vramn1402.
18. Tkacheva ON, Kotovskaya YuV, Aleksanyan LA, et al. Novel coronavirus infection SARSCoV-2 in elderly and senile patients: prevention, diagnosis and treatment. Expert Position Paper of the Russian Association of Gerontology and Geriatrics. Cardiovascular Therapy and Prevention. 2020;19(3):2601. (In Russ.) doi:10.15829/1728-8800-2020-2601.
About the Authors
M. M. LukyanovRussian Federation
Moscow
S. Yu. Martsevich
Russian Federation
Moscow
A. A. Pulin
Russian Federation
Moscow
N. P. Kutishenko
Russian Federation
Moscow
E. Yu. Andreenko
Russian Federation
Moscow
V. P. Voronina
Russian Federation
Moscow
V. A. Dindikova
Russian Federation
Moscow
N. A. Dmitrieva
Russian Federation
Moscow
A. V. Zagrebelny
Russian Federation
Moscow
A. N. Makoveeva
Russian Federation
Moscow
O. V. Lerman
Russian Federation
Moscow
E. Yu. Okshina
Russian Federation
Moscow
А. S. Sgibneva
Russian Federation
Moscow
A. A. Smirnov
Russian Federation
Moscow
E. N. Belova
Russian Federation
Moscow
V. G. Klyashtorny
Russian Federation
Moscow
E. V. Kudryashov
Russian Federation
Moscow
O. E. Karpov
Russian Federation
Moscow
O. M. Drapkina
Russian Federation
Moscow
Supplementary files
Review
For citations:
Lukyanov M.M., Martsevich S.Yu., Pulin A.A., Kutishenko N.P., Andreenko E.Yu., Voronina V.P., Dindikova V.A., Dmitrieva N.A., Zagrebelny A.V., Makoveeva A.N., Lerman O.V., Okshina E.Yu., Sgibneva А.S., Smirnov A.A., Belova E.N., Klyashtorny V.G., Kudryashov E.V., Karpov O.E., Drapkina O.M. Dynamics of age characteristics and prevalence of concomitant cardiovascular and non-sardiovascular diseases in patients hospitalized with COVID-19 during epidemic wave: data from TARGET-VIP registry. Cardiovascular Therapy and Prevention. 2021;20(8):3106. https://doi.org/10.15829/1728-8800-2021-3106

























































