Scroll to:
Quality of medication therapy in patients after stroke depending on presence/absence of diabetes: data from the outpatient stage of REGION-M registry
https://doi.org/10.15829/1728-8800-2021-2856
Abstract
Aim. To assess the quality of medication treatment in the polyclinic within 2 years after discharge, depending on presence/absence of diarecommended for patients with stroke before its development and betes.
Material and methods. The study included 684 patients assigned to the City Polyclinic № 64 (Moscow), discharged from F.I. Inozemtsev City Clinical Hospital (Moscow) for a period from January 1, 2012 to April 30, 2017 with a diagnosis of stroke/transient ischemic attack, of which 122 were diagnosed with diabetes.
Results. Before stroke, therapy was recommended for 67,3% of patients with diabetes and 54,7% without diabetes (p<0,01): statins — 15,5 and 14,4%, antiplatelet agents — 32,7 and 25,5%, angiotensinconverting enzyme (ACE) inhibitors/angiotensin II receptor blockers (ARBs) — 41,4 and 37,9%, beta-blockers (BBs) — 9,1% and 7,8%, respectively. For the first 6 months after stroke, the rate of statin therapy increased to 39,6 and 39,2%, antiplatelet drugs — to 62,6 and 51,9%, ACE inhibitors/ARBs — to 68,2 and 66%, BBs — to 51,6 and 37,2%, respectively. Then, after 6 months it decreased again to 28,8 and 27,1% for statins, to 30,7 and 35,2% for antiplatelet agents, to 43,3 and 42,6% for ACE inhibitors/ARBs and remained the same for BBs, respectively. There were no significant differences in the prevalence of prescribing most drugs to patients with and without diabetes, both before and after stroke, with the exception of hypoglycemic medications.
Conclusion. The therapy of patients with previous stroke, both with and without diabetes, recommended in the polyclinic, is characterized by an insufficient prescription rate of main drug classes necessary for secondary cardiovascular prevention at all follow-up stages.
For citations:
Martsevich S.Yu., Tolpygina S.N., Zagrebelny A.V., Chernysheva M.I., Voronina V.P., Kutishenko N.P., Dmitrieva N.A., Lerman O.V., Lukina Yu.V., Blagodatskikh S.V., Lukyanov M.M., Okshina E.Yu., Parsadanyan N.E., Drapkina O.M. Quality of medication therapy in patients after stroke depending on presence/absence of diabetes: data from the outpatient stage of REGION-M registry. Cardiovascular Therapy and Prevention. 2021;20(5):2856. https://doi.org/10.15829/1728-8800-2021-2856
Introduction
Stroke is the predominant cause of disability in the population [1][2]. Stroke survivors have an unfavorable life prognosis, primarily due to the high risk of cardiovascular events (CVEs) and recurrent strokes. Thus, stroke risk increases by ~10 times in persons who had ischemic stroke and transient ischemic attack (TIA), while it is highest in the early disease stages. Secondary prevention of CVEs should begin as early as possible after the development of stroke and should be carried out throughout the rest of life [3-5] in accordance with international guidelines for secondary prevention of ischemic stroke [5][6].
One of the significant risk factors for stroke and its unfavorable outcomes is diabetes [1][7][8]. According to recent studies, more than 10% of patients with type 2 diabetes die as a result of stroke [9], and a significant part of these patients die in the acute stage. In patients with diabetes, the risk of CVEs is extremely high, and CVE prevention should also be carried out continuously [7-8]. The peculiarities of treatment of stroke patients with and without diabetes at the outpatient stage remain insufficiently studied. In this publication, for the first time, an analysis of medication therapy prescribed in an outpatient clinic to patients with stroke within 12 months before and two years after its development is presented in the outpatient stage of REGION-M registry.
Evidence-based medicine data indicate that early initiation of secondary CVE prevention in persons who have undergone stroke can significantly reduce the risk of recurrent MI [4-9]. Considering the high social significance of stroke, investigation of drug treatment quality in routine outpatient practice in patients with/ without diabetes is important.
The aim was to assess the quality of medication treatment in the polyclinic recommended for patients with stroke before its development and within 2 years after discharge, depending on presence/absence of diabetes.
Material and methods
The protocol of the entire REGION registry and its individual parts was published in detail earlier [10-12]. In this fragment of the study, we used data from the outpatient part of REGION-M registry, which included all patients assigned to the City Polyclinic № 64 (Moscow), discharged from the F.I. Inozemtsev City Clinical Hospital (Moscow) in the period from January 1, 2012 to April 4, 2017 with stroke or TIA.
On the basis of the polyclinic № 64 electronic database, 684 attached patients were identified who were discharged from the hospital during the above-mentioned period with stroke/TIA. Among them there were 122 patients with diabetes and 562 without diabetes. The diagnosis of diabetes without type specification in the outpatient part of the registry was established based on its presence in the patient’s outpatient card. Socio-demographic characteristics, clinical and history data, type of stroke, risk factors (RF), cardiovascular (CVD) and concomitant diseases, results of visits to outpatient physicians and prescribed medications for the last 12 months before the event, for the first 6 months after it and at the last visit. The median follow-up was 22 (interquartile range, 13,0- 37,75) months. The quality of medication therapy was assessed based on its compliance with modern clinical guidelines for treatment and prevention of CVEs in patients with stroke and diabetes mellitus who visit outpatient clinics [6][7].
Statistical analysis was performed using the SPSS Statistics version 23.0 software package (IBM, USA). Variables are presented as absolute numbers and percentage of the total. Differences between groups of patients were determined using the Pearson χ2 test with Yates’ correction. Differences were considered significant at p<0,05.
Results
In the cohort of patients with stroke and diabetes, the mean age of patients (M±SD) and the proportion of women were significantly higher compared with patients with stroke without diabetes: 71,5±10,9 vs 68,0±14,7 years (р<0,05) and 72,1 vs 55,2% (p<0,05), respectively. Depending on the type of stroke, the patients with and without diabetes did not differ significantly. The proportion of TIA was 10,7 vs 18,7%, ischemic stroke — 82,0 vs 73,7%, hemorrhagic stroke — 6,9 vs 7,4% (p>0,05), mixed ischemic and hemorrhagic stroke — 0,6 and 0,2%. Figure 1 presents data on prevalence of CVDs and concomitant diseases in patients included in the outpatient part of REGION-M registry with and without diabetes. Persons with concomitant diabetes compared with those without diabetes were significantly more likely to have prior coronary artery disease (CAD) (p<0,001), prior myocardial infarction (MI) (p<0,001), stroke (p<0,05), chronic kidney disease (CKD) (p<0,001) and heart failure (HF) (p<0,001). Hypertension (HTN) was noted in the majority of patients with stroke. However, in patients with diabetes it was detected significantly more often as follows: 95,9% vs 81,3%, respectively (p<0,001).
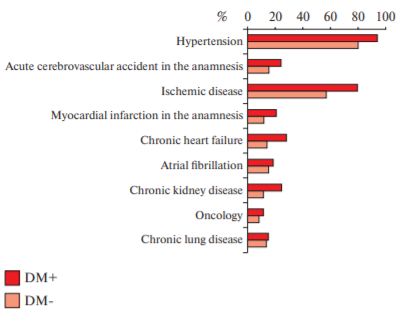
Figure 1. The presence of CVDs and comorbidities in stroke patients with and without diabetes.
Note: CPD — chronic pulmonary disease.
There was no data on such RFs as smoking, obesity, hyperlipidemia, sedentary lifestyle, positive family history for early CVDs, and alcohol abuse in the vast majority of outpatient records. A comparison of RF prevalence in the groups of patients with and without diabetes was carried out.
Since the quality of therapy was assessed according to outpatient records, a comparative analysis of main clinical, history and demographic characteristics of patients who visited and did not visited the polyclinic at different follow-up stages was carried out. Patients with diabetes were observed by doctors more often than without diabetes: 90,2 vs 81,7% (p<0,05) before the stroke, 74,6 and 61,7% (p<0,001) within 6 months after stroke, and in the period from 6 months to the end of follow-up period — 85,2 and 76,9%, respectively (p<0,01). Before stroke, there were more visits of comorbid patients with diabetes 19 vs 10% without diabetes (p<0,05), or with disability — 38,5 vs 11,3% (p<0,001), prior stroke — 20,2 vs 5,2% (p<0,001), CAD — 69 vs 26% (p<0,001), HF — 17 vs 6% (p<0,01), atrial fibrillation (AF) — 18 vs 8,7% (p<0,05), HTN — 92 vs 45% (p<0,001), CKD — 16,5 vs 2,6% (p<0,001), cancer — 10,4 vs 4,3% (p<0,01). Patients who visited a polyclinic after stroke were also more likely to have disabilities, diabetes and comorbidities.
Next, we analyzed the prescription rate of medication therapy to patients after stroke at different followup stages and its compliance with modern clinical guidelines [6-8]. Since nootropic, antioxidant and other neurotropic drugs do not have a strong evidence base regarding the improving prognosis of patients after stroke, they were not included in the analysis.
Table 1 shows the prescription rate of various drug groups before stroke in patients with diabetes (n=110) and without it (n=459) who visited a polyclinic within 12 months before stroke. There were no significant differences in prescription rate of various drug groups in people with and without diabetes, with the exception of hypoglycemic agents. Prior to hospitalization, drugs in a polyclinic were recommended to 67,3% of patients with diabetes and 54,7% of patients without diabetes (p<0,01), although the former visited a polyclinic sig - nificantly more often — 90,2 vs 81,7% (p<0,05). Statins were prescribed to only 15,5% of patients with diabetes and 14,4% without it, antiplatelet agents — 32,7 and 25,5%, angiotensin converting enzyme (ACE) inhibitors/angiotensin II receptor blockers (ARBs) — 41,4 and 37,9%, beta-blockers (BB) — 9,1 and 7,8%, respectively.
Table 1
Prescription rate of various drug groups before hospitalization (within 12 months before the reference stroke) in patients with and without diabetes (n=569)
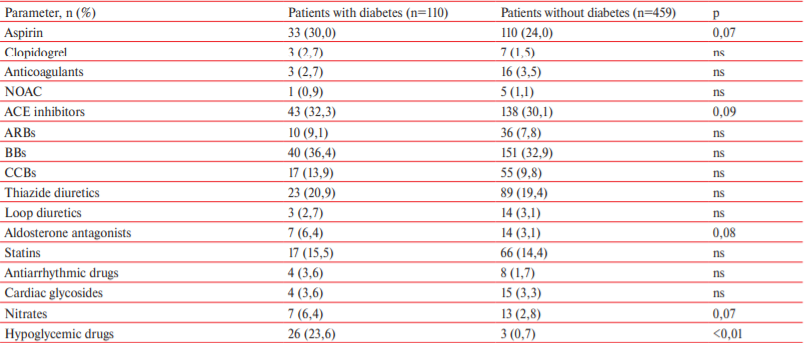
Note: ns — not significant.
Considering that the majority of patients had a high CVE risk even before stroke, the prescription rate of the main drug groups reducing CVE risk was extremely low. Thus, out of 112 patients with AF, only 19 (17%) received oral anticoagulants (warfarin or novel oral anticoagulants (NOACs)) before the stroke. According to an analysis, 61,8% of patients had CAD, 92% — hypertension, 17,8% — diabetes, while only 17% received statins before the stroke. The situation with antiplatelet agents (aspirin and clopidogrel) was no better — 18% of patients received it, while no less than 62% should have received it. In the presence of hypertension in 92% of patients, only 40% and 15% received ACE inhibitors/ARBs and BBs before the reference stroke, respectively.
Table 2 shows the prescription rate of various drug groups by outpatient physicians after hospitalization in 438 patients (with diabetes, n=91; without diabetes, n=347) who appeared in the polyclinic within the first 6 months after stroke. Patients with diabetes significantly more often than those without concomitant diabetes were prescribed with hypoglycemic drugs, clopidogrel, BBs, and calcium channel blockers (CCBs). In relation to other drug classes, no significant differences were found. As in the prehospital stage, the prescription rate of main drug groups indicated for secondary prevention of CVD was insufficient. Thus, the prescription rate of antiplatelet agents/anticogulants and statins did not exceed 60-70 and 40% in both groups, respectively.
Table 2
Prescription rate of various drug groups after hospitalization (first 6 months after stroke) in patients with and without diabetes (n=438)
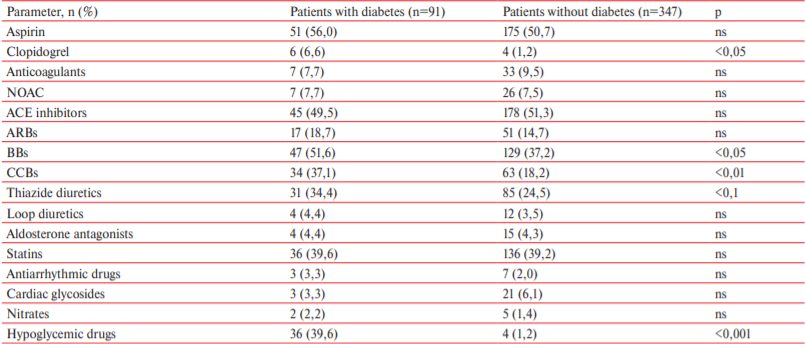
Note: ns — not significant.
Table 3 shows the prescription rate of various drug groups in the polyclinic in 536 patients with (n=104) and without (n=432) diabetes ≥6 months after the reference stroke until the end of follow-up period. There were no significant differences in the prescription rate in subgroups of patients with and without diabetes. At the same time, there was a decrease in prescription rate of antiplatelet agents and statins 6 months after the stroke compared with the first 6-month follow-up. Aspirin was prescribed in 56% and 50,7% of patients with and without diabetes, respectively, in the first 6 months and only 26,9% and 33% of patients with and without diabetes, respectively after 6 months (p<0,05 for both groups), and statins — 39,6% of patients with diabetes and 39,2% without diabetes in the first 6 months and 28,8% of patients with diabetes and 27% without diabetes after 6 months (p<0,05 for both groups).
Table 3
Prescription rate of various drug groups after hospitalization (6 months after stroke) in patients with and without diabetes (n=536)
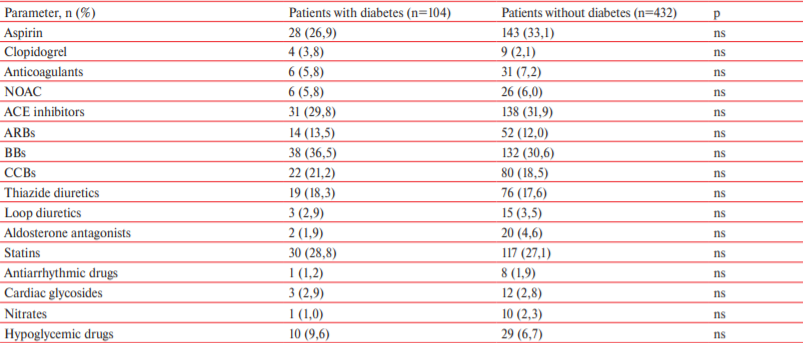
Note: ns — not significant.
Discussion
Since the assessment of therapy prescribed by outpatient physicians at different follow-up stages was carried out based on the ambulatory medical records of patients who visited the polyclinic before and/or after the reference stroke, we analyzed the incidence of outpatient visits. IIt was found that the same number of patients visited polyclinic during the last 12 months before and after the event as follows: 90% — patients with diabetes, 83% — patients without diabetes. An indepth analysis showed that mainly patients with diabetes or disability, as well as those with other chronic diseases, visited the polyclinic, i.e. the most severe patients.
The fact that more than half of the patients who had a high CVE risk before stroke due to the presence of diabetes, CVDs, such as CAD, AF, HF, HTN and previous MI, did not receive adequate medication therapy, and that there were no data on RFs and bad habits in the overwhelming majority of outpatient records, indicates the insufficient attention of outpatient doctors to primary and secondary prevention of CVEs. These patients should have received at least statins, antiplatelet agents or anticoagulants, ACE inhibitors/ ARBs, and BBs. So, at the time of stroke development, only ~17% of patients received statins, ~18% — antiplatelet agents, 40% — ACE inhibitors/ARBs, 15% — BBs, which is clearly not enough. A similar situation was found in the LIS-2 registry, where only a small proportion of patients received outpatient treatment prior to reference stroke [13]. The presence of diabetes practically did not affect the quality of primary and secondary prevention of CVDs at the prehospital stage, although in persons with diabetes, the management of RFs should be carried out more intensely [7][8].
After reference stroke, the prescription rate of medication therapy in the polyclinic for the first 6 months after stroke significantly increased both in the group of patients with and without diabetes for statins, antiplatelet agents, ACE inhibitors/ARBs and BBs. However, it still remained insufficient. Six months after discharge, the prescription rate of medication therapy in the groups with and without diabetes decreased by 50 and 33%, respectively, for statins, by 30 and 35% for antiplatelet agents, by 40 and 31% for ACE inhibitors/ARBs (p<0,05), and remained the same for BBs.
There were no significant differences in the prescription rate of most drug groups to patients with and without diabetes, both before and after reference stroke, with the exception of hypoglycemic agents at all stages, and more frequent prescription of BBs, CCBs and clopidogrel to patients with diabetes in the first 6 month after discharge.
Thus, a significant part of patients with a very high CVE risk did not receive the entire set of drugs necessary for secondary CVE prevention. In the available literature, we did not find publications that would provide data on outpatient treatment of patients after stroke, aimed at secondary prevention of MI and other CVEs. Similar trends were identified in the PROGNOZ IBS register, where there was an increase in the prevalence of using antiplatelet drugs, statins, BBs, ACE inhibitors/ARBs in patients with stable CAD discharged from the hospital after coronary angiography, and its subsequent decrease after 4 and 7 years of follow-up [14].
The importance of secondary prevention in patients after stroke is showed by the Russian clinical study [15] conducted by neurologists involved in outpatient rehabilitation of patients after stroke. The authors found a significant difference in the mortality rate among patients who received effective secondary prevention of CVEa, both without (refusal of bad habits, increasing physical activity, losing weight) and with medication. Most (n=281) patients underwent effective prevention of recurrent MI. Only a small part (45 out of 326) of patients refused regular therapy, despite a doctor’s recommendation. Death from stroke, MI, or vascular events developed in 5% of patients who took regular treatment, and in 47% of patients who did not constantly take antihypertensive drugs or antiplatelet drugs after stroke. Men, smokers, and alcohol abusers were reliably more likely to refuse from taking medications on a regular basis. In the group of patients after ischemic stroke who regularly took treatment, recurrent stroke (3 and 16%, respectively), MI (1 and 7%), death from CVDs (1 and 13,8%) developed much less frequently than in patients who did not receive regular therapy.
Conclusion
The therapy of patients with previous stroke, both with and without diabetes, recommended in the polyclinic, is characterized by an insufficient prescription rate of main drug classes necessary for secondary cardiovascular prevention at all follow-up stages.
Relationships and Activities: none.
References
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics 2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146-603. doi:10.1161/CIR.0000000000000485.
2. Medical and demographic indicators of the Russian Federation in 2017: Stat. Directory/Ministry of Health of Russia. M, 2018. 264 c. (In Russ.)
3. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160-236. doi:10.1161/STR.0000000000000024.
4. Lau G, Pendlebury S, Rothwell P. Long-Term Prognosis after Transient Ischemic Attack and Stroke. In Transient Ischemic Attack and Stroke: Diagnosis, Investigation and Treatment. Cambridge: Cambridge University Press. 2018;253-64. doi:10.1017/9781316161609.018.
5. Sacco RL, Adams R, Albers G, et al. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association Council on Stroke: Co-Sponsored by the Council on Cardiovascular Radiology and Intervention: The American Academy of Neurology affirms the value of this guideline. Stroke. 2006;37:577-617. doi:10.1161/01.str.0000199147.30016.74.
6. European Stroke Organization (ESO) Executive Committee; ESO Writing Committee. Guidelines for management of ischemic stroke and transient ischemic attack. Cerebrovasc Dis. 2008;25:457-507. doi:10.1159/000131083.
7. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur Heart J. 2020;41:255-323. doi:10.1093/eurheartj/ehz486.
8. Dubinina II, Zhadnov VA, Yankina SV, et al. Risk factors and features of cerebral vessel damage in type 2 diabetes mellitus in combination with cerebrovascular disease. Russian Medical and Biological Bulletin named after Academician I.P. Pavlov. 2012;3:104. (In Russ.)
9. Skvortsova VI, Shetova IM, Kakorina EP, et al. Reduction in stroke death rates through a package of measures to improve medical care for patients with vascular diseases in the Russian Federation. The Russian Journal of Preventive Medicine. 2018;21(1):4-10. (In Russ.)
10. Boytsov SA, Martsevich SYu, Kutishenko NP, et al. The study “Register of Patients after Acute Stroke (REGION)”. Part 1. Hospital Prospective Register of Patients after Acute Stroke (According to the Results of the Pilot Phase of the Study). Rational Pharmacotherapy in Cardiology. 2016;12(6):645-53. (In Russ.)
11. Martsevich SY, Kutishenko NP, Lukyanov MM, et al. The study “Hospital register of patients with acute cerebrovascular accident (REGION)”: characteristics of patient and outcomes of hospital treatment. Cardiovascular Therapy and Prevention. 2018;17(6):32-8. (In Russ.)
12. Voronina VP, Zagrebelnyi AV, Lukina YuV, et al. Features of cerebral stroke course in patients with diabetes mellitus according to the REGION-M register. Cardiovascular Therapy and Prevention. 2019;18(5):60-5. (In Russ.)
13. Boytsov SA, Martsevich SY, Ginzburg ML, et al. Lyubertsy study on mortality rate in patients after cerebral stroke or transient ischemic attack (LIS-2). Design and medical treatment estimation. Rational Pharmacotherapy in Cardiology. 2013;9(2):114-22. (In Russ.)
14. Tolpygina SN, Polyanskaya YuN, Martsevich SYu. Treatment of patients with chronic ischemic heart disease in real clinical practice according to the data from PROGNOZ IBS register (part 2) Rational Pharmacotherapy in Cardiology. 2013;9(5):494-9. (In Russ.)
15. Parfenov VA, Verbitskaya SV. Secondary prevention of ischemic stroke: international recommendations and clinical practice. Neurology J. 2014;2:4-10. (In Russ.)
About the Authors
S. Yu. MartsevichRussian Federation
Moscow.
S. N. Tolpygina
Russian Federation
Moscow.
Tel.: +7 (906) 793-92-63
A. V. Zagrebelny
Russian Federation
Moscow.
M. I. Chernysheva
Russian Federation
Moscow.
V. P. Voronina
Russian Federation
Moscow.
N. P. Kutishenko
Russian Federation
Moscow.
N. A. Dmitrieva
Russian Federation
Moscow.
O. V. Lerman
Russian Federation
Moscow.
Yu. V. Lukina
Russian Federation
Moscow.
S. V. Blagodatskikh
Russian Federation
Moscow.
M. M. Lukyanov
Russian Federation
Moscow.
E. Yu. Okshina
Russian Federation
Moscow.
N. E. Parsadanyan
Russian Federation
Moscow.
O. M. Drapkina
Russian Federation
Moscow.
Supplementary files
Review
For citations:
Martsevich S.Yu., Tolpygina S.N., Zagrebelny A.V., Chernysheva M.I., Voronina V.P., Kutishenko N.P., Dmitrieva N.A., Lerman O.V., Lukina Yu.V., Blagodatskikh S.V., Lukyanov M.M., Okshina E.Yu., Parsadanyan N.E., Drapkina O.M. Quality of medication therapy in patients after stroke depending on presence/absence of diabetes: data from the outpatient stage of REGION-M registry. Cardiovascular Therapy and Prevention. 2021;20(5):2856. https://doi.org/10.15829/1728-8800-2021-2856
JATS XML

























































