Scroll to:
Contribution of hypertension and other risk factors to survival and mortality in the Russian population
https://doi.org/10.15829/1728-8800-2021-3003
Abstract
Aim. To study the contribution of hypertension (HTN) to survival and mortality in the Russian population.
Material and methods. This prospective observational cohort included representative samples from 11 Russian regions (men and women aged 25-64 years, n=18251) examined in 2012-2014 as part of the Epidemiology of Cardiovascular Diseases and their Risk Factors in Regions of Russian Federation (ESSE-RF) study. The examination included a questionnaire (12 modules), anthropometric and blood pressure (BP) measurements, as well as biochemical blood tests. HTN was considered aa a systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg, or when a subject receives antihypertensives. Treatment efficacy was considered as the proportion of persons (%) who achieved target BP among those taking antihypertensives. Depending on HTN status, all participants were divided into 4 groups: 1) those without HTN;
2) those with HTN, taking antihypertensive agents and having systolic BP ≤140 mm H. and diastolic BP ≤90 mm Hg (effective therapy);
3) those with HTN, taking medications, but not achieving target BP (ineffective therapy); 4) those with HTN, not taking antihypertensives. The life status of participants was updated every 2 years. Kaplan-Meier survival curves, as well as univariate and multivariate Cox proportional hazards models were created.
Results. The presence of HTN significantly reduced survival (p<0,001) in the cohort, which is significant when adjusted for age (men — relative risk (RR)=1,47, p<0,001, women — RR=1,17, p<0,001). In the multivariate model, the male sex (RR=2,3 p<0,001), age increase, smoking, tachycardia, and HTN are significant for all-cause mortality only for men, but not for women. However, for women, absence of higher education was significant. The presence of HTN significantly worsens cardiovascular survival in both sexes (p<0,0001). HTN increases the risk of a composite endpoint for both men and women (p<0,001). Analysis of Kaplan-Meier curves showed the worst survival rate in persons with HTN, taking antihypertensive drugs, but not reaching target BP levels.
Conclusion. The presence of HTN significantly worsens the survival rate of men and women. Special attention of medical community should be directed to increasing the proportion of effectively treated patients with HTN.
For citations:
Balanova Yu.A., Shalnova S.A., Kutsenko V.A., Imaeva A.E., Kapustina A.V., Muromtseva G.A., Evstifeeva S.E., Maksimov S.A., Karamnova N.S., Yarovaya E.B., Kulakova N.V., Kalachikova O.N., Chernykh T.M., Belova O.A., Artamonova G.V., Indukaeva E.V., Grinshtein Yu.I., Libis R.A., Duplyakov D.V., Rotar O.P., Trubacheva I.A., Serebryakova V.N., Efanov A.Yu., Konradi A.O., Boytsov S.A., Drapkina O.M. Contribution of hypertension and other risk factors to survival and mortality in the Russian population. Cardiovascular Therapy and Prevention. 2021;20(5):3003. https://doi.org/10.15829/1728-8800-2021-3003
Introduction
In the modern world, hypertension (HTN) is a global public health problem. In the presence of modern diagnosis and treatment methods, an unsolved problem is still insufficient treatment coverage and failure to achieve target blood pressure (BP) [1-3]. HTN is not only a medical, but also a significant economic problem, being not only an independent disease, but also a risk factor (RF) for noncommunicable diseases (NCDs). The economic impact of HTN, caused by its contribution to morbidity and mortality from NCDs in Russia, in 2016 amounted to more than RUB 869936 million [4].
International and Russian guidelines emphasize the need for early detection of HTN and aggressive BP reduction to the target level. Countries with better BP control, such as Austria, Germany, Finland and France, have the lowest deaths due to stroke. The reverse situation is observed in countries where BP is less controlled — in Hungary, Belarus, and the Baltic countries. This problem is also relevant in Russia, where less than a quarter of those with HTN controls the BP level [3][5]. As shown by a meta-analysis that included randomized placebo-controlled trials, a BP decrease by 10 mm Hg reduces the stroke risk by 27%, coronary artery disease (CAD) — by 17%, heart failure — by 28% and all-cause death — by 17% [6].
Studying the contribution of BP levels and HTN status to mortality, along with other factors, is important. To understand the contribution of RF to mortality, Russian researchers are interested in the data from domestic studies investigating Russian cohorts. Traditionally, serious epidemiological work is carried out by Siberian scientists. Within the World Health Organization (WHO) project Monitoring trends and determinants in Cardiovascular disease (MONICA) from 1984-85 to 1994-95, a cohort study was carried out in Novosibirsk, where the HTN prevalence was studied depending on BP levels and the 10-year cardiovascular death risk was assessed. The analysis showed that among hypertensive patients, the death risk increases from lower BP levels to higher ones. In addition, Simonova GI et al. (2006) [7] showed the higher cardiovascular death risk among men, which may be due to better BP control among female cohort. Twelve-year prospective follow-up including representative sample of Tyumen residents aged 25- 64 years by Akimova EV et al. (2013) [8] showed that the relative risk (RR) of cardiovascular death increases from systolic BP (SBP) levels ≥141 mm Hg and diastolic blood pressure (DBP) ≥86 mm Hg. The risk of cardiovascular events is significantly increased in women with SBP ≥152 mm Hg and DBP ≥95 mm Hg. An increased SBP compared to DBP makes a more significant contribution to the attributive cardiovascular death risk. A 26-year follow-up of a Moscow cohort, carried out within at the National Medical Research Center for Therapy and Preventive Medicine, revealed that people with increased SBP live less than those with normal SBP: men − by 12,2 years, women − by 12,3 years; increased DBP has a slightly lower values — 8,5 and 6,4 years, respectively [9]. At the same time, to reduce the death risk at population level, a significant role is played not so much by antihypertensive therapy, as by the achievement of target BP levels. Dolgalev I.V. et al. (2019) conducted a 27-year cohort prospective study including Tomsk residents (men, 630; women, 916 people aged 20-59 years), which studied the effect of hypertension, smoking and a combination of these factors on mortality. HTN has a significant effect on all-cause mortality (RR=2,2) both for men (RR=1,89) and women (RR=2,54). In combination with smoking, the all-cause risk doubles [10]. The sample consists of Ryazan residents from the MERIDIAN-RO cohort prospective study (n=1622, 36-month follow-up). Filippov EV et al. (2019) analyzed the relationship between RFs and outcomes and indicated the HTN as most significant effect among other RFs on composite endpoint (all-cause death + nonfatal ischemic stroke + nonfatal myocardial infarction (MI) [11].
It is common knowledge that cohort studies are extremely difficult and laborious. Contacting with individuals in a cohort, establishing their life status and presence of fatal or non-fatal events, is a painstaking and multicomponent work that requires sufficient funding. Therefore, most of studies carried out in Russia analyzes data from one region. The Epidemiology of Cardiovascular Diseases and their Risk Factors in Regions of Russian Federation (ESSE-RF) study is a unique project, which allows to receive data from prospective observation of 11 Russian regions.
Thus, the aim was to study the contribution of HTN to survival and mortality in the Russian population.
Material and methods
The material was representative samples of the population from 11 Russian regions aged 25-64 years, studied in 2012-2014 as part of the ESSE-RF study.
In the ESSE-RF study, a systematic stratified multistage community-based sample was used, formed by the Kish method. The sampling methodology has been described in detail earlier [12]. The response rate was ~80%. The study was approved by the Ethics Committees of following federal centers: National Medical Research Center for Therapy and Preventive Medicine; Almazov National Medical Research Center; National Medical Research Center of Cardiology. All participants signed written informed consent.
The respondents were interviewed using an original modular questionnaire (12 modules) based on adapted international methods. It contains information on sociodemographic characteristics, economic living conditions, behavioral habits, and history data. After a 5-minute rest, BP was measured on the right hand with an automatic BP monitor Omron M3 Expert (Japan) in a sitting position. BP was measured twice with an interval of ~2-3 min. During analysis, the average of two measurements was used. HTN was diagnosed at a SBP ≥140 mm Hg and/or DBP ≥90 mm Hg, or when taking antihypertensive therapy. Proportion of persons (%) who achieved target BP values among those taking antihypertensives was considered treatment efficacy.
All subjects were divided into 4 groups depending on HTN status:
1) Subjects without HTN;
2) Subjects with HTN, taking antihypertensives and having SBP ≤140 mm Hg and DBP ≤90 mm Hg (effective treatment);
3) Subjects with hypertension who do not take antihypertensives;
4) Subjects with hypertension, taking medications, but not reaching target BP levels (ineffective treatment).
The analysis included sex, age, income level, educational level (higher, secondary, below secondary), rural/urban area, alcohol abuse (>168 g per week of ethanol for men and >84 g per week for women), smoking (never/former/current smoking), obesity (body mass index ≥30 kg/m2), abdominal obesity (AO) (waist circumference ≥102 cm for men and ≥88 cm for women), lipid profile (high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL C), triglycerides (TGs), as well as a history of type 2 diabetes (T2D), MI, and stroke. An unfavorable lipid profile (dyslipidemia) was diagnosed at following levels: HDL-C ≤1,0/1,2 mmol/L for men/women, respectively, LDL-C ≥3,0 mmol/L and TG ≥1,7 mmol/L.
A cohort for prospective observation was formed from the subjects. A cohort included representative samples from 11 Russian regions (n=18251; age, 25-64 years). The life status of each subject was assessed once every 2 years (Figure 1). The data was collected by each participated region and transmitted to the federal center. With the help of healthcare centers, territorial compulsory medical insurance funds or personal (telephone) contact, information was collected on non-fatal events (cardiovascular events and new CVD cases). The death causes were established through the territorial compulsory medical insurance funds, the Rosstat department (death certificates), medical and preventive centers, personal (telephone) contact with the family of subjects. In the event of death, the cause was coded according to International Classification of Diseases (ICD-10).

Figure 1. Prospective observation scheme.
Over the 6-year follow-up period, 393 (2,2%) people died, of which 141 people died from CVDs: CAD — 82 subjects, stroke — 39 subjects. Contact with 274 (1,5%) subjects was unavailable.
Statistical analysis was performed using the R 3.6.1 environment. The Kaplan-Meier survival curves were used to estimate the survival probability at a certain time point. Comparison of two survival curves was carried out using the logrank test. When comparing three or more survival curves, the Holm correction for multiple comparisons was applied. The Cox proportional hazards model (Cox regression) was used to predict all-cause and cardiovascular risk or the risk of adverse events (CAD, including MI, stroke, revascularization, or cardiovascular death) and to assess the effect of predetermined independent variables on this risk. Differences were significant at p<0,05.
Results
We analyzed the survival rate among Russian population, depending on presence of hypertension. The Kaplan-Meier survival curves in HTN presence were significantly lower in comparison with the curves without it, both among men (p<0,0001) and women (p<0,001) (Figure 2). Age-adjusted Cox model confirmed significance of HTN for both men (RR=1,47, p<0,001) and women (RR=1,17, p<0,001).

Figure 2. Survival depending on hypertension presence among men and women aged 25-64 years in Russia.
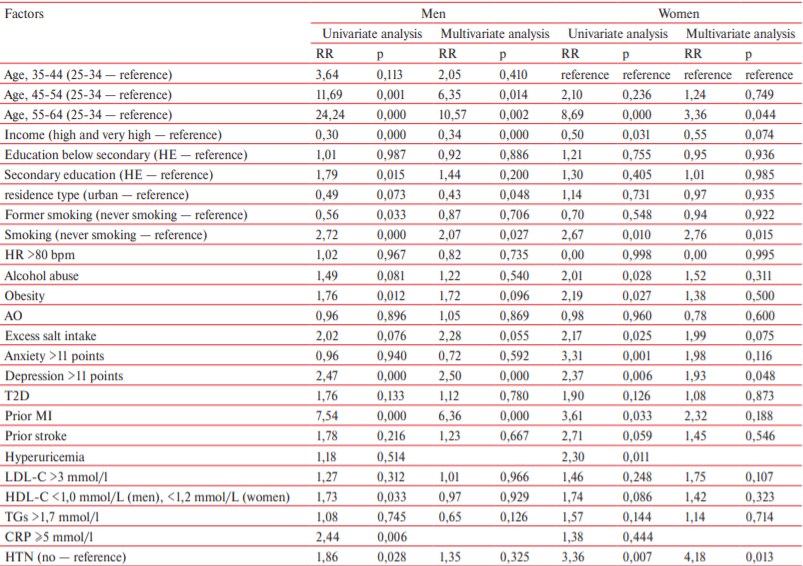
To understand the place of HTN among other factors for all-cause mortality, an analysis was performed using a proportional hazards model (Table 1). There were following significant factors for the Russian population: male sex (RR=2,3 p<0,001), older age, no higher education (HE) (education below secondary was insignificant, possibly due to low number of people in the group). Among behavioral RFs, current smoking was significant, while for men, former smoking. Alcohol abuse was insignificant.
Table 1
RR of all-cause mortality among men and women aged 25-64 in Russia (Cox model)

Note: HR — heart rate.
Noteworthy is the significance of tachycardia both for men (RR=2,07, p<0,001) and for women (RR=1,69, p<0,001). A significant contribution was made by current/prior diseases — MI, stroke, anxiety, while in women — T2D and depression, in men — AO. Among biochemical parameters, hyperuricemia and hypertriglyceridemia are significant for women, and elevated levels of LDL-C and C-reactive protein (CRP) for men.
In the multivariate model, CRP and hyperuricemia were excluded, since its assessment was performed in all regions. In this model, the significance of education, prior stroke and former smoking disappears for men, while current smoking remains significant. The presence of HTN also remained significant for men, but not for women. For women, in multivariate analysis, the significance of higher education absence appeared, but anxiety and T2D became insignificant.
HTN significantly worsens cardiovascular survival in both sexes (p<0,0001) (Figure 3).

Figure 3. Cardiovascular survival depending on hypertension presence among men and women aged 25-64 years in Russia (p<0,0001).
In the Cox proportional hazards model, the relationship between HTN and other factors affecting cardiovascular mortality was analyzed (Table 2). Among women aged 25-34 years, no deaths were noted, while women aged 25-44 years became the reference group. Male sex remains significant (RR=2,88, p<0,001) even to a greater extent than for all-cause mortality. In women, the following factors became additionally significant for cardiovascular mortality: rural residence, obesity and hypertriglyceridemia. For men, anxiety and stroke became insignificant. At the same time, significant positive relationships between HTN and cardiovascular mortality were revealed for both sexes.
Table 2
RR of cardiovascular mortality among men and women aged 25-64 in Russia
Note: HR — heart rate.
Multivariate analysis showed the lower significance of age. For men, residence in urban areas, no high income, current smoking, tachycardia and prior stroke remain significant. Interestingly, the presence of HTN became insignificant. For women, smoking, tachycardia and, as before, HTN remain significant for cardiovascular mortality.
We also studied contribution of HTN to composite endpoint, which included cardiovascular death, as well as non-fatal events (MI and stroke). Survival curves for men and women with HTN were significantly lower than those for non-hypertensive subjects (p<0,0001) (Figure 4). The presence of HTN increased the risk of composite endpoint for both men and women (p<0,001). Moreover, this effect was more pronounced than on all-cause and cardiovascular mortality — ageadjusted Cox model leaves HTN significant both for men (RR=1,57, p<0,001) and for women (RR=2,38, p<0,001).

Figure 4. Survival depending on hypertension presence taking into account non-fatal endpoints among men and women aged 25-64 years in Russia (p<0,0001).
For a more in-depth analysis, Kaplan-Meier curves were created depending on HTN status for allcause and cardiovascular mortality. The survival curve in non-hypertensive men (Figure 5 A, red curve) was significantly higher than in those with HTN. Survival curves for subjects not taking antihypertensive therapy (blue curve) and being treated effectively (green curve) are below the red curve, but do not differ from each other. The worst survival rate was in hypertensive subjects with ineffective treatment (purple curve). In women, the survival curves were gentler. However, in women, ineffective treatment significantly worsens survival (Figure 5 B).
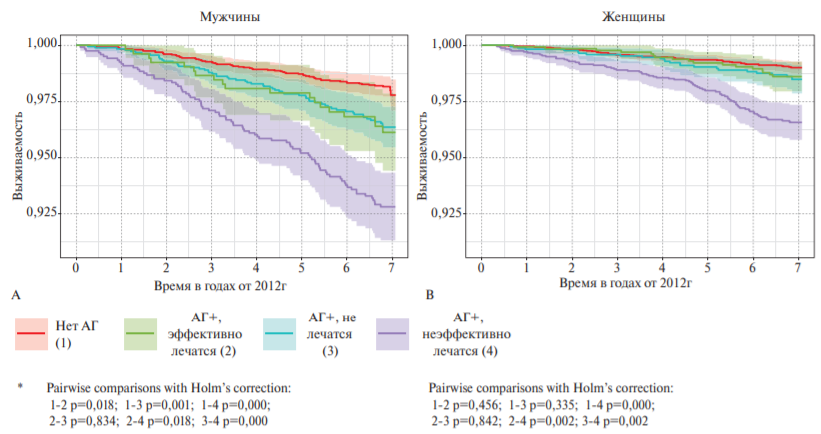
Figure 5. Survival depending on HTN status among men (A) and women (B) aged 25-64 years in Russia*.
Note: * — differences of curves: women, all with the 4; men, no difference only between 2 and 3
1-2 p=0,018; 1-3 p=0,001; 1-4 p=0,000; 2-3 p=0,834; 2-4 p=0,018; 3-4 p=0,000
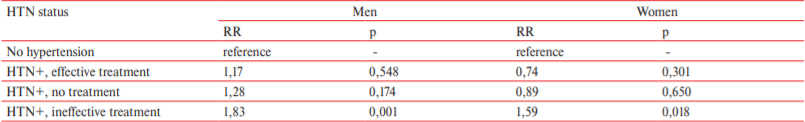
After analysis using Cox proportional hazards models adjusted for age, only the group of ineffective treatment remained significantly associated with allcause, regardless of age (Table 3).
Table 3
RR of total mortality depending on HTN status among men and women aged 25-64 years in Russia (age-adjusted Cox model)
Discussion
The growing burden of NCDs in Russia, as in many countries of the world, causes an increase in health care system costs. The interest in HTN from the medical community is not accidental. HTN in Russian is one of the most common and significant diseases [3, 5]. In addition, it is one of important modifiable CVD RFs [13]. Comprehensive study of HTN is an important component of strategy to reduce mortality in Russia. Hypertension characteristics can be studied by epidemiological research with prospective observation. The contribution of BP to life expectancy decrease in Russian population is very high. In the Moscow cohort, it is more than 12 years for SBP [9]. In addition, significance of HTN for increasing all-cause and cardiovascular mortality is demonstrated by regional studies, performed in Tomsk, Novosibirsk, and Ryazan [7][10][11]. The study carried out in Shanghai from 2002 to 2020 with 223097 hypertensive patients demonstrated that the incidence of cardiovascular events in this cohort is influenced by age increase, HTN grade and duration of the disease [14].
Current analysis has demonstrated that HTN significantly worsens survival rates in Russia, including cardiovascular, and emphasized the role of HTN not only as a disease, but also as a powerful NCD RF. The risk of non-fatal cardiovascular events in the presence of HTN is also increased. The survival curves depending on HTN status deserve special attention, since the category of ineffectively treated patients has significantly lower rates in comparison with those who are effectively treated and not treated at all.
In Russia, after two significant jumps in the mortality rate observed in 1990-1993 in 1998-2003, there is a gradual decrease. As noted by Boytsov SA et al. (2018), this decrease was largely due to a decrease in cardiovascular mortality [15]. Despite the increase in prevalence of HTN in Russia, over a 20-year period, the treatment coverage of hypertensive patients and its effectiveness increased significantly [5]. During the period from conduction of Federal Target Program “Prevention and Treatment of HTN in Russia”, the proportion of people with high BP (≥160/95 mm Hg) has decreased, mainly due to the female part of population; the proportion of people who control BP among hypertensive subjects increased from 14,9 to 23,1% [3][5]. A decrease in the population BP level and an improvement in HTN control can significantly contribute to a decrease in cardiovascular mortality, which has been demonstrated in the Czech population [16]. The role of SBP reduction in significant decrease of CVD and all-cause death risk is reflected in a systematic review with meta-analysis by Bundy JD, et al. (2017), where the minimum risk was observed at a SBP level of 120-124 mm Hg [17]. In addition, the significance of HTN control for reducing cardiovascular mortality is reflected in the study by Brunström M, et al. (2018) [18]. In the systematic review with meta-analysis, Sakima A, et al. (2019) showed that reaching BP <130/80 mm Hg is associated with a significant reduction in major cardiovascular events [19]. In a Moscow cohort aged >55 years, observed at the National Medical Research Center for Therapy and Preventive Medicine, a significant association of elevated BP, especially among those receiving treatment, with all-cause and cardiovascular mortality was shown [20].
Thus, the Russian medical community faces a large and difficult task — increasing the proportion of effectively treated people among those with HTN and, as a result, an increase in the number of those who control BP. At the moment, in Russia, among all persons with HTN, about half of those receiving antihypertensive therapy are effectively treated, and only every seventh man and every fourth woman controls BP [3][5], while in the USA and Canada — 71 and 82%, respectively [21]. The factors associated with ineffective HTN treatment in Russia were analyzed in detail in the study by Shalnova SA et al. [22] and allowed to describe the profile of such patients — these are elderly obese patients who abuse alcohol more often (both men and women). They have tachycardia 2 times more often. The impact on these RFs at the population level is also a significant resource for increasing HTN control in Russia, which provides an additional resource for reducing mortality. With a significant decrease in survival in the presence of HTN, the doctor’s special attention should be focused on ineffectively treated patients, which can be resolved within the dispensary follow-up.
Relationships and Activities: none.
#Regional ESSE-RF study participants who collected and processed data from cross-sectional and prospective fragments of the ESSE-RF study: Vologda: Ilyin V.A., Kalashnikov K.N., Popov A.V.; Voronezh: Bondartsov L.V., Furmenko G.I.; Vladivostok: Mokshina M.V., Nevzorova V.A., Rodionova L.V., Shestakova N.V.; Ivanovo: Romanchuk D.V., Shutemova E.A.; Krasnoyarsk: Baikova O. A., Danilova L. K., Evsyukov A.A., Kosinova A.A., Petrova M.M., Ruf R.R., Shabalin V.V., Filonenko I.V.; St. Petersburg: Baranova E.I.; Tomsk: Karpov R.S., Kaveshnikov V.S.; Tyumen: Storozhok M.A., Shalaev S.V.; Kemerovo: Barbarash O.L., Danilchenko Ya.V., Mulerova T.A., Tabakaev M.V.
References
1. Shalnova SA, Deev AD, Balanova YuA, et al. Twenty years trends of obesity and arterial hypertension and their association in Russia. Cardiovascular Therapy and Prevention. 2017;16(4):4-10. (In Russ.)
2. Shalnova SA, Deev AD, Balanova YuA. Treatment of hypertension in patients at high risk. Monotherapy or combination? Lechaschij vrach. 2016;7:17-23. (In Russ.)
3. Boytsov SA, Balanova YuA, Shalnova SA, et al. Arterial hypertension among individuals of 25-64 years old: prevalence, awareness, treatment and control. By the data from ECCD. Cardiovascular Therapy and Prevention. 2014;14(4):4-14. (In Russ.)
4. Balanova YuA, Kontsevaya AV, Myrzamatova AO, et al. Economic Burden of Hypertension in the Russian Federation. Rational Pharmacotherapy in Cardiology. 2020;16(3):415-23. (In Russ.)
5. Balanova YuA, Shalnova SA, Imaeva AE, et al. Prevalence, Awareness, Treatment and Control of Hypertension in Russian Federation (Data of Observational ESSERF-2 Study). Rational Pharmacotherapy in Cardiology. 2019;15(4):450-66. (In Russ.)
6. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The Lancet. 2016;387(10022):957-67. doi:10.1016/S0140-6736(15)01225-8.
7. Simonova G, Nikitin Yu, Glushanina O, et al. Arterial hypertension and the risk of cardiovascular mortality in an urban Siberian population. The Siberian Scientific Medical Journal. 2006;4(122):88-92. (In Russ.)
8. Akimova EV, Pushkarev GS, Gafarov VV, et al. Risk of cardiovascular death in relation to blood pressure levels in Tyumen men and women: results of a 12-year prospective study. Terapevticheskii Arkhiv. 2013;85(3):70-4. (In Russ.)
9. Konstantinov VV, Deev AD, Balanova IuA, et al. The cardiovascular risk profile and its contribution to survival in Moscow men and women aged 35-64 years. Profilakticheskaya Meditsina. 2013;16(1):3-7. (In Russ.)
10. Dolgalev IV, Brazovskaya NG, Ivanova AYu, et al. Influence of arterial hypertension, smoking, and their combination on mortality (according to the results of a 27-year cohort prospective study of the unorganized population of Tomsk). Russian Journal of Cardiology. 2019;(1):32-7. (In Russ.)
11. Filippov EV, Vorobyev AN, Dobrynina NV, et al. Adverse cardiovascular outcomes and their relationship with risk factors according to the prospective study MERIDIAN-RO. Russian Journal of Cardiology. 2019;(6):42-8. (In Russ.)
12. Research Organizing Committee of the ESSE-RF project. Epidemiology of cardiovascular diseases in different regions of Russia (ESSE-RF). The rationale for and design of the study. The Russian Journal of Preventive Medicine. 2013;16(6):25-34. (In Russ.)
13. Danaei G, Lu Y, Singh GM. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Lancet Diabetes & Endocrinology. 2014;2(8):634-47.
14. Li Al, Zhu S, Hu Zh, et al. The distribution and epidemic characteristics of cerebrovascular disease in followed-up hypertension patients. Sci Rep 2021;11:9366. doi:10.1038/ s41598-021-88127-5.
15. Boytsov SA, Shalnova SA, Deev AD. Cardiovascular mortality in the Russian Federation and possible mechanisms of its changes. Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova. 2018;118(8):98-103. (In Russ.)
16. Ci'fkova R, Skodova Z, Bruthans J, et al. Longitudinal trends in cardiovascular mortality and blood pressure levels, prevalence, awareness, treatment, and control of hypertension in the Czech population from 1985 to 2007/2008. J Hypertens. 2010;28(11):2196-203.
17. Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2(7):775-81. doi:10.1001/jamacardio.2017.1421.
18. Brunstrom M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels a systematic review and meta-analysis. JAMA Intern Med. 2018;178(1):28-36. doi:10.1001/jamainternmed.2017.6015.
19. Sakima A, Satonaka H, Nishida N, et al. Optimal blood pressure targets for patients with hypertension: a systematic review and meta-analysis. Hypertension Research. Hypertension Res. 2019;42(4):483-95. doi:10.1038/s41440-018-0123-4.
20. Imaeva AE, Balanova YA, Kapustina AV, et al. Associations between blood pressure and mortality among middle-aged and elderly men and women: a Cohort Study. Ekologiya cheloveka [Human Ecology]. 2020;9:49-56. (In Russ.)
21. Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a crosssectional study. BMJ Open. 2013;3:e003423. doi:10.1136/ bmjopen-2013-003423.
22. Shalnova SA, Konradi AO, Balanova YuA, et al. What factors do influence arterial hypertension control in Russia? Cardiovascular Therapy and Prevention. 2018;17(4):53-60. (In Russ.)
About the Authors
Yu. A. BalanovaРоссия
Moscow.
Tel.: +7 (916) 283-61-42
S. A. Shalnova
Россия
Moscow.
V. A. Kutsenko
Россия
Moscow.
A. E. Imaeva
Россия
Moscow.
A. V. Kapustina
Россия
Moscow.
G. A. Muromtseva
Россия
Moscow.
S. E. Evstifeeva
Россия
Moscow.
S. A. Maksimov
Россия
Moscow.
N. S. Karamnova
Россия
Moscow.
E. B. Yarovaya
Россия
Moscow.
N. V. Kulakova
Россия
Vladivostok.
O. N. Kalachikova
Россия
Vologda.
T. M. Chernykh
Россия
Voronezh.
O. A. Belova
Россия
Ivanovo.
G. V. Artamonova
Россия
Kemerovo.
E. V. Indukaeva
Россия
Kemerovo.
Yu. I. Grinshtein
Россия
Krasnoyarsk.
R. A. Libis
Россия
Orenburg.
D. V. Duplyakov
Россия
Samara.
O. P. Rotar
Россия
St. Petersburg.
I. A. Trubacheva
Россия
Tomsk.
V. N. Serebryakova
Россия
Tomsk.
A. Yu. Efanov
Россия
Tyumen.
A. O. Konradi
Россия
St. Petersburg.
S. A. Boytsov
Россия
Moscow.
O. M. Drapkina
Россия
Moscow.
On behalf of the ESSE-RF study participants#
Review
For citations:
Balanova Yu.A., Shalnova S.A., Kutsenko V.A., Imaeva A.E., Kapustina A.V., Muromtseva G.A., Evstifeeva S.E., Maksimov S.A., Karamnova N.S., Yarovaya E.B., Kulakova N.V., Kalachikova O.N., Chernykh T.M., Belova O.A., Artamonova G.V., Indukaeva E.V., Grinshtein Yu.I., Libis R.A., Duplyakov D.V., Rotar O.P., Trubacheva I.A., Serebryakova V.N., Efanov A.Yu., Konradi A.O., Boytsov S.A., Drapkina O.M. Contribution of hypertension and other risk factors to survival and mortality in the Russian population. Cardiovascular Therapy and Prevention. 2021;20(5):3003. https://doi.org/10.15829/1728-8800-2021-3003
JATS XML

























































