ADDRESS TO THE READERS
CORONARY HEART DISEASE
What is already known about the subject?
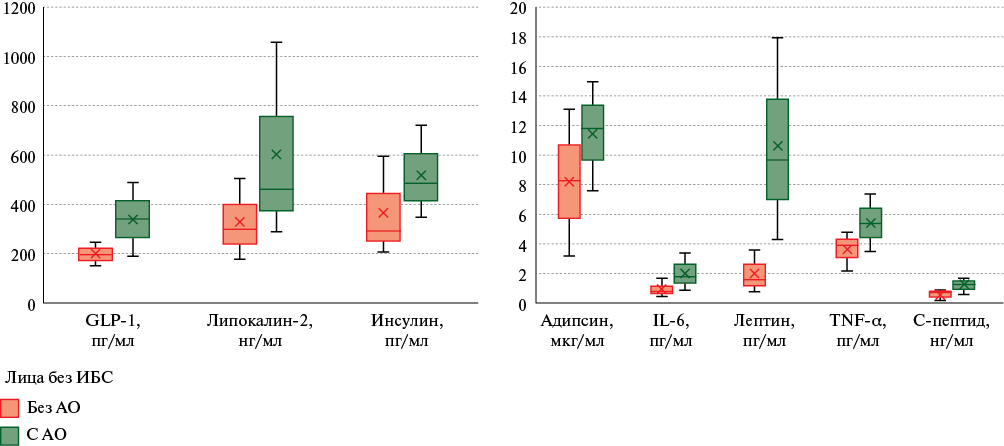
- Visceral adipose tissue is an independent hormone-producing organ synthesizing biologically active substances (adipokines).
- There is a high prevalence of abdominal obesity in the world, the presence of which is associated with coronary artery disease.
What might this study add?
- In young people, premature coronary artery disease is associated with increased blood levels of adiponectin, resistin and cholesterol, which is not part of high-density lipoproteins.
- In young people with abdominal obesity, premature coronary artery disease is associated with increased serum levels of plasminogen activator inhibitor 1.
Aim. To evaluate the associations of abdominal obesity (AO), adipokines and premature coronary artery disease (CAD) in young people for a deeper understanding of the pathogenesis of atherosclerotic diseases.
Material and methods. A total of 1457 people were examined, including 653 (44,8%) men. Mean age was 36,7±6,0 years. Premature CAD was detected in 46 people, while 4 following subgroups were formed (138 people in total): with CAD and AO; with CAD, without AO; control groups by age and sex: without CAD, with AO; without CAD, without AO.
Results. Premature CAD in young people is associated with an increase in non-high-density lipoprotein cholesterol (non-HDL-C). Univariate analysis found that the probability of CAD increased by 1% with an increase in adiponectin level, and by 0,2% with an increase of 1 ng/ml in resistin level. Multivariate regression analysis, including sex, age, waist circumference, non-HD-C, adiponectin, and resistin, significant associations were obtained for non-HDL-C and adiponectin. With AO, the CAD probability increased by 0,6% with an increase in plasminogen activator inhibitor-1 level (PAI-1). However, when non-HDL-C was included in the model, significance for this biomarker was not achieved.
Conclusion. In young people, CAD is associated with increased levels of non-HDL cholesterol, adiponectin, resistin and PAI-1. Independent associations with premature CAD were obtained only for adiponectin, which makes this marker promising for study in young people.
What is already known about the subject?
- Thousands of papers are published annually on the diagnosis and treatment of coronary artery disease (CAD), but between various professional medical societies there are no uniform approaches and criteria on how to use International Classification of Diseases codes related to chronic CAD.
What might this study add?
- There is no agreed upon interpretation of chronic coronary artery disease codes among practitioners, which contributes to the distortion of morbidity and mortality statistics based on the International Classification of Diseases (10threvision) codes.
Aim. To study the opinion of doctors about the applicability, frequency and criteria for practical use of codes of the International Classification of Diseases, 10th revision (ICD-10) from the group of chronic coronary artery disease (CAD) — I25.0, I25.1, I25.8, I25.9.
Material and methods. This cross-sectional study was conducted in the period from February 27, 2024 to March 11, 2024 on a continuous sample of medical workers who agreed to participate in an anonymous survey as respondents. The questionnaire consisted of an introductory, personal and main part, which consisted of 19 questions devoted to various aspects of chronic CAD coding at the doctor’s appointment and during preparing medical death certificate. This article presents the results of a survey of cardiologists (group 1) and internists/general practitioners/family physicians (group 2). The χ2 test was used to compare two groups. The Friedman test was used to test the hypothesis that the physicians' opinion about the use of different chronic CAD codes was random. The Kendall test was used to assess the agreement between physicians. Calculations were carried out using Microsoft Office Excel 2021 and SPSS-26.0.
Results. A total of 883 doctors from 47 constituent entities of the Russian Federation took part in the survey. Half of the respondents believed that there are differences between the codes I25.0, I25.1, I25.8, I25.9 and that they are necessary for statistical recording. Although cardiologists (59,2%) were less likely than internists/general practitioners/family doctors (65,9%) to believe that one or more of the 4 codes analyzed could be used only on the basis of risk factors, differences did not reach significance (p=0,1). The need to confirm chronic CAD using paraclinical research methods varied from 57,3% for code I25.9 to 83,1% for code I25.1. In case of death of a patient from chronic CAD, almost a third of respondents do not see the differences between the 4 specified codes, but are ready to use them in different clinical setting. In addition, 14,6% responded that when filling out medical death certificates they would not use any of the 4 specified codes. There is no agreement among physicians regarding the use of codes in clinical practice (Kendall's coefficient of concordance 0,084; p<0,001) and as a cause of death (0,148; p<0,001).
Conclusion. There is no unified stance among doctors on the rules and applicability of using at least 4 codes (I25.0, I25.1, I25.8, I25.9). To correctly assess morbidity and mortality rates from individual forms of chronic ACAD based on ICD-10 codes, guidelines that should include a description and consideration of all the most significant clinical scenarios of chronic CAD should be developed.
MYOCARDIAL INFARCTION
What is already known about the subject?
- Studies conducted in the pre-reperfusion era of acute myocardial infarction (MI) treatment have shown that the prognosis after recurrent MI is significantly worse than after primary MI.
What might this study add?
- Long-term follow-up of patients after a acute MI in 2017 who received modern therapy showed that the death risk of patients after a recurrent MI continues to be very high and significantly exceeds the risk of patients with a primary MI.
Aim. To compare the long-term prognosis of life of patients after primary and recurrent acute myocardial infarction (MI).
Material and methods. The study was based on the RIMIS registry, which included all patients after transmural MI in 2017 in one of the Moscow vascular centers. The prospective part included 191 patients who survived the acute stage of MI, of which 145 suffered a primary acute MI, 46 — a recurrent acute MI. Long-term follow-up data were collected 71 (53;75) months after discharge from the hospital. The primary endpoint was any-cause death.
Results. During the follow-up period, 35 (25,2%) patients with a primary MI and 25 (64,1%) patients with a recurrent MI died (p<0,001). It was not possible to establish the fate of 13 (6,81%) patients, of which 7 (4,83%) were people with primary MI and 6 (13,04%) people with recurrent MI. The death risk was significantly higher in patients who had a recurrent MI compared to patients who had a primary MI: hazard ratio (HR)=3,52 (2,09;5,96), p<0,001). An unfavorable prognosis was determined not by the fact of a recurrent MI, but by the complications that resulted from a previous MI, primarily heart failure, as well as age, sex, smoking status, and hospitalizations for cardiovascular diseases in the year before the reference MI, history of angina and following comorbidities: a prior stroke, major bleeding (life-threatening gastrointestinal bleeding requiring complex surgical intervention). Patients who had a recurrent MI were significantly more adherent to follow-up and prescribed therapy.
Conclusion. Despite the modern strategy for treating MI both in the acute stage and in the long-term period, the prognosis after recurrent MI remains unfavorable. Signs negatively affecting the prognosis were sex, age, a history of heart failure and angina pectoris, and hospitalizations for cardiovascular diseases one year prior to reference MI.
CARDIOVASCULAR RISK FACTORS
What is already known about the subject?
- Globally, there has been an increase in the incidence of both type 2 diabetes (T2D) and prediabetes, which is an established risk factor for diabetes.
What might this study add?
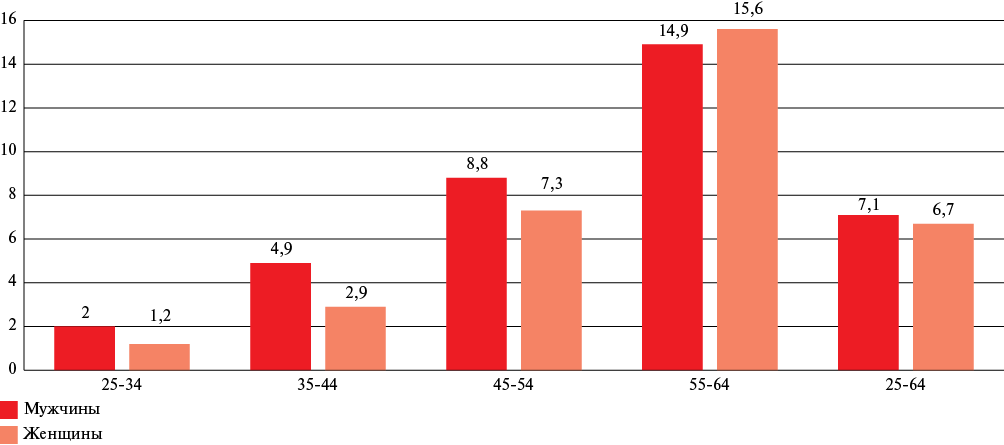
- The prevalence of T2D in the Russian population aged 25-64 years was 6,9% (men — 7,1%, women — 6,7%), while the prevalence of prediabetes (based on impaired fasting glycemia) was 6,2% (men — 7,7%, women — 5,0%).
- Multivariate analysis adjusted for sex, age and region demonstrated that T2D, but not impaired fasting glycemia, significantly decreases survival and increases the composite endpoint rate in the Russian Federation.
Aim. To assess the prevalence of type 2 diabetes (T2D) and prediabetes in the Russian population aged 25-64 years, as well as the association of prediabetes with risk factors (RFs) of noncommunicable disease. To study the contribution of carbohydrate metabolism disorders to mortality and the occurrence of cardiovascular events.
Material and methods. We included data from cross-sectional studies ESSE-RF and ESSE-RF2. The final sample included 26418 people (10268 men and 16150 women) who signed informed consent. A modular questionnaire was used. Biochemical parameters were determined in the National Medical Research Center for Therapy and Preventive Medicine with an Abbott Architect c8000 autoanalyzer using diagnostic kits from Abbott Diagnostics (USA). Impaired fasting glycemia (IFG) was defined as a fasting plasma glucose concentration of 6,1-6,99 mmol/L. The presence of T2D was determined by interview and/or fasting plasma glucose ≥7,0 mmol/L. Obesity was defined as a body mass index of ≥30,0 kg/m2. Abdominal obesity was defined as a waist circumference of ≥102 cm in men and ≥88 cm in women. A prospective observation cohort was formed from 14 regions of ESSE-RF and ESSE-RF2 (n=22812). The vital status of each examined person was clarified once every 2 years. Information on fatal and non-fatal events was collected. Statistical processing was performed using the open-source statistical programming language and R environment (version 4.1). Associations were assessed using logistic regression. Kaplan-Meier curves were used to estimate survival. Associations with endpoints were assessed using Cox proportional hazards models.
Results. In the Russian population aged 25-64 years, the prevalence of T2D and prediabetes, assessed by IFG, was 6,9% (men — 7,1%, women — 6,7%) and 6,2% (men — 7,7, women — 5,0% (p<0,001)), respectively. Age, low level of education, obesity, including abdominal obesity, hypertension, tachycardia, hyperuricemia and lipid metabolism disorders were significantly associated with prediabetes, and for men, additionally, stress. Prediabetes and T2D demonstrated a significant decrease of survival, including cardiovascular survival, and the occurrence of a composite endpoint. However, multivariate analysis adjusted for sex, age, and region of residence indicates a significant contribution of T2D, but not IFG.
Conclusion. To reduce the T2D burden in the Russian Federation, patients with T2D should be identified early and RFs should be controled. Early detection of prediabetes plays a significant role in the prevention of T2D. In addition, T2D and prediabetes have common risk factors, and therefore common ways of prevention.
What is already known about the subject?
- The influence of meteorological factors, especially changes in their parameters, on human health is multifaceted and ambiguous.
- Rapid changes in ambient temperature can increase morbidity, mortality, and hospitalization.
What might this study add?
- Negative air temperatures in a metropolis are associated with an increase in hospitalizations for symptomatic blood pressure increase, arrhythmias such as atrial fibrillation, or decompensated heart failure.
Many patients and some doctors associate the worsening of cardiovascular diseases with meteoropathy (changes in atmospheric pressure and air temperature). Opinion about lack of weather influence on the increase in overall morbidity and the lack of related research data indicate the need to study the relationship between cardiovascular diseases and meteorological conditions.
Aim. To assess the prevalence of hospitalizations with symptomatic increases in blood pressure (BP), atrial fibrillation (AF), and decompensated heart failure (HF) in a Moscow hospital depending on meteorological conditions.
Material and methods. This retrospective analysis of the number of emergency hospitalizations of patients with symptomatic increases in blood pressure, AF, and decompensated HF in Moscow City Clinical Hospital № 24 was carried out in the period from October 1, 2018 to September 30, 2019. Information from the website www.weather.com was used as a source of meteorological data. The following indicators were assessed daily: daytime air temperature (t), nighttime air temperature, maximum diurnal air temperature variation, atmospheric pressure, maximum diurnal atmospheric pressure variation, amount of precipitation. To assess statistical significance, the Mann-Whitney and Kruskal-Wallis tests were used. A correlation analysis was carried out, and a prognostic model was created using multiple linear regression.
Results. During the period from October 1, 2018 to September 30, 2019, 4354 patients were hospitalized at City Clinical Hospital № 24 with symptomatic BP increase and/or AF and/or decompensated HF. The highest number of hospitalizations occurred in November, December and January. The median number of admissions per day was 12 patients. When comparing the mean number of patients admitted to the hospital per day, depending on day- and nighttime air temperature, following statistically significant differences were obtained (p<0,001): with day- and nighttime air temperature ≥0о C, the number of admissions was less compared to sub-zero temperatures. Significant inverse correlations were established between the number of patients hospitalized with symptomatic BP increase, AF and HF per day, with air temperature at night (correlation coefficient r=-0,339; p<0,001), air t during the day (r=-0,316; p<0,001), temperature difference over 48 hours (r=-0,205; p<0,001); direct correlations with atmospheric pressure (r=0,106; p=0,044) and its changes (r=0,115; p=0,028) were identified. All identified relationships were of moderate strength. According to prognostic model, only nighttime air temperature turned out to be a significant indicator associated with the hospitalization rate per day. With a decrease in air temperature at night for every 7,5о C <0, one more patient is expected to be hospitalized with a symptomatic BP increase, decompensated HF, or paroxysmal AF.
Conclusion. Negative air temperature in a metropolis is associated with an increase in hospitalizations for symptomatic BP increase, AF or decompensated HF. Atmospheric pressure and precipitation do not affect these conditions.
What is already known about the subject?
- Every tenth adult in the world experiences at least one depressive episode during their lifetime. According to epidemiological studies, the prevalence of depressive disorders in cardiac patients exceeds 20%.
- Increased interest in cognitive impairment in depression is due to significant changes in ideas about the etiology and pathogenesis of depression. Cognitive disorders are a multifactorial syndrome that occurs in many cardiac diseases.
What might this study add?
- Associations of depression with cognitive impairment (patterns of memory, attention and thinking) in persons 25-44 years old were determined.
- Associations have been established for the depression presence depending on sex and level of education and cognitive impairment (patterns of memory, attention and thinking) among people aged 25-44 years.
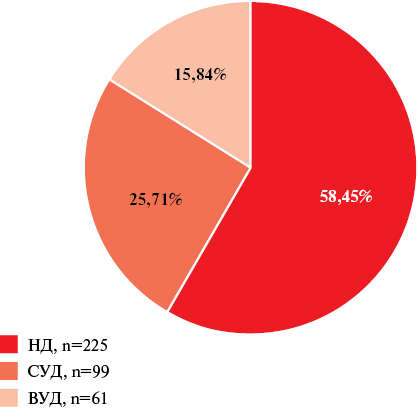
Aim. To establish associations between the depression level as an independent cardiovascular risk factor and cognitive impairment (patterns of memory, attention and thinking) in people aged 25-44 years.
Material and methods. In 2013-2016, a random representative sample of people aged 25-44 years was studied in one of the Novosibirsk districts. A total of 463 men (mean age 35,94±5,96 years) and 546 women (mean age 36,17±5,99 years) were examined. Standardized tests were used to assess cognitive function. Depression level was assessed according to the MOPSY (MONICA-psychosocial) World Health Organization program criteria.
Results. In the surveyed random representative sample of people aged 25-44 years, the prevalence of higher education was the highest (60,5%). The depression prevalence in women was higher than in men: high depression level — 15,84 and 8,64%; the mean depression level was 25,71 and 21,3%, respectively. Univariate analysis showed that the attention stability according to the dot cancellation test at a moderate and high depression level was reduced only in men with higher education, compared with those without depression (p=0,018). In persons of both sexes with secondary professional education in a random representative sample of persons aged 25-44 years, associations between depression and memory pattern disturbances were identified. In the resulting multivariate model, men in a random representative sample of persons aged 25-44 years without depression did not have any cognitive impairment in patterns of memory, attention and thinking.
Conclusion. An association has been established between the depression and cognitive impairment (patterns of memory, attention and thinking) in people aged 25-44 years.
ИССЛЕДОВАНИЯ В КАРДИОЛОГИИ
What is already known about the subject?
- Patients who successfully undergo percutaneous coronary angioplasty have restenosis more often than other adverse outcomes.
- Implantation of drug-eluting stents does not guarantee protection against in-stent restenosis.
What might this study add?
- In patients with stable coronary artery disease, vascular endothelial growth factor-A (VEGF-A) promotes angiogenesis in the stented segment, thereby promoting drug-eluting in-stent restenosis.
- A significant plasma increase in VEGF-A within 24 hours after stent implantation is associated with angiographic in-stent restenosis in the long-term period.
The introduction of drug-eluting stents (DES) into clinical practice has led to a significant reduction in the incidence of in-stent restenosis (ISR) compared to implantation of bare metal stents. However, in 2-4% of cases, the development of angiographic restenosis is observed. Vascular Endothelial Growth Factor-A (VEGF-A) promotes early endothelialization of the stented segment, but in some cases can promote progressive neointimal growth due to proinflammatory effects.
Aim. To evaluate the influence of plasma VEGF-A level on ISR after DES implantation.
Material and methods. We prospectively examined 49 patients who were implanted with DES due to stable coronary artery disease with ischemia-related arterial stenosis >70% according to a stress test, as well as with a fractional flow reserve <0,8. Plasma VEGF-A level was assessed immediately before the procedure and 24 hours after it. The follow-up period was 11±4 months from the moment of intervention. Subsequently, all study participants underwent repeated coronary angiography to determine whether they had angiographic ISR and to identify patients at risk of recurrent angina pectoris. In 9 patients (18% of participants), angiographic ISR was recorded in the long-term period.
Results. The groups of patients with and without long-term restenosis were comparable in terms of initial VEGF-A levels: 481 (259; 674) and 560 (339; 766) pg/ml, respectively (p>0,05). Within 24 hours after stent implantation, a significant increase in VEGF-A level was found in patients who subsequently demonstrated angiographic ISR as follows: from 476 (267; 602) to 1117 (1089; 1573) pg/ml (p<0,05). A positive moderate correlation was established between the plasma VEGF-A content 24 hours after stent implantation and angiographic ISR in the long-term period (r=0,55; p<0,001).
Conclusion. Initial plasma VEGF-A levels are not associated with angiographic ISR. Moreover, a sharp increase in VEGF-A level f within 24 hours after coronary stenting is associated with drug-eluting ISR.
CLINIC AND PHARMACOTHERAPY
What is already known about the subject?
- Ischemic heart disease is associated with an inadequate blood supply to the myocardium due to closure of the arteries by atherosclerotic plaques.
- The mechanism of adenosine diphosphate P2Y12receptor antagonists by their receptor binding activity that activates the G-protein inhibitor secondary messenger system, mediates the completion and amplification of the aggregatory responses.
What might this study add?
- Dyspnea is evident in patients who received ticagrelor.
- Clopidogrel (irreversible P2Y12inhibitor) is superior to the ticagrelor (reversible P2Y12antagonist).
- In Iraqi patients, the cost is the major issue that led to ticagrelor discontinuation.
In patients with chronic coronary syndrome, ticagrelor decreases cardiovascular events more efficiently than clopidogrel. In several studies investigating novel P2Y12 inhibitors dyspnea has been detected. A rise of adenosine blood levels is supposed to be one of cases of dyspnea induced by ticagrelor. Dyspnea is a prevalent and complex symptom. It is associated with deterioration of the quality of life and hospital readmission.
Aim. To determine the frequency of dyspnea related with ticagrelor or clopidogrel intake in patients with stable coronary artery disease undergoing coronary intervention. Also, to determine which patients could continue ticagrelor intake and which patients couldn’t, and show the causes of ticagrelor discontinuation.
Material and methods. Between October 2023 and January 2024, an observational prospective comparative case-control study was conducted at Baghdad Heart Center in Baghdad Teaching Hospital in Medical City. In this study, individuals with stable coronary artery disease who just had therapeutic catheterization and dual antiplatelet therapy were included. The patients from group 1 received aspirin and ticagrelor, while those from group 2 received aspirin and clopidogrel.
Results. A total of 120 patients were included. With the ticagrelor intake, the severity of dyspnea was classified as mild 64.2% (77 [120]) and moderate 19.1% (23 [120]). About 16.7% (20 [120]) had no dyspnea at all. The difference between patients who continued ticagrelor intake (16%) and those who stopped using it (84%) was significant. With clopidogrel intake no dyspnea was recorded.
Conclusions. According to our findings, the risk or occurrence of dyspnea is only evident in patients who received ticagrelor. When compared to irreversible P2Y12 inhibitors like clopidogrel, the reversible P2Y12 antagonist ticagrelor has a higher incidence of dyspnea in increasing order.
What is already known about the subject?
- Recurrent venous thromboembolism occurs in 10% of high-risk patients within the first year after the initial episode and reaches 30% by 5-year follow-up.
- The most effective prevention method of recurrent venous thromboembolism is long-term anticoagulant therapy.
What might this study add?
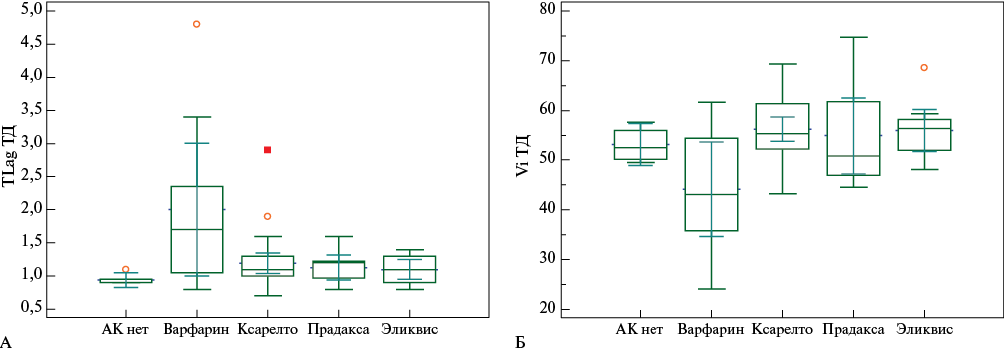
- Reduction of the bleeding risk during long-term anticoagulant therapy is possible by coagulation monitoring using integral methods, such as the thrombin generation test and thrombodynamics.
- Direct oral anticoagulation therapy led to an effective clot growth delay, while the endogenous thrombin potential did not reach a critically low level compared with warfarin therapy.
Aim. To determine differences in laboratory coagulation parameters using routine and integral monitoring methods in patients depending on anticoagulant therapy >12 months after pulmonary embolism (PE) with a high recurrence risk.
Material and methods. The study included 72 patients who, according to indications, received long-term anticoagulant therapy >12 months due to a high risk of recurrent thromboembolism. During the follow-up period (15-20 months from the first pulmonary embolism episode), the plasma coagulation parameters were studied using a conventional panel and D-dimer assessment, as well as a thrombin generation test and thrombodynamics. Patients adherent to prolonged anticoagulation were included in group 1. During the collection period, 8 patients independently stopped taking anticoagulants, despite the high risk of recurrent pulmonary embolism (group 2).
Results. There were no significant differences in coagulation parameters and D-dimer levels between the studied groups of patients. In the group of patients continuing to take anticoagulants, there was an increase in clot growth delay parameters in comparison with patients of group 2 according to the thrombodynamics results (p=0,046) and the thrombin generation test in platelet-poor plasma in comparison with reference values (p=0,001).
Conclusion. Long-term anticoagulant therapy effectively prevents recurrent venous thromboembolism. In patients after primary pulmonary embolism who refuse anticoagulation, the clot growth delay values are shortened, which indicates an increased risk of recurrent venous thromboembolism. The most stable plasma coagulation parameters are observed in patients taking direct oral anticoagulants.
CLINICAL CASE
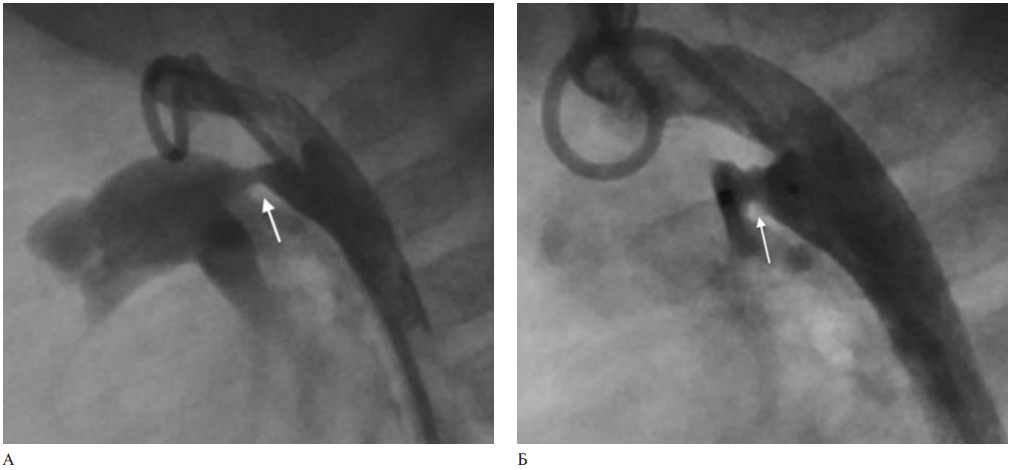
- A case series of intravascular ultrasound (IVUS) use in X-ray endovascular surgery of congenital heart defects is described.
- IVUS helps in assessing the vessel morphology and determining the vessel lumen area after angioplasty.
- IVUS in combination with angiography helps to evaluate in more detail the anatomy of the patent ductus arteriosus and to more correctly select a device for occlusion.
Intravascular imaging methods are an actively developing area that was originally used in the treatment of coronary artery disease. With the help of intravascular ultrasound (IVUS), there is an opportunity to more objectively, in contrast to fluoroscopy, evaluate the vascular anatomy and lesion morphology, as well as optimize transcatheter interventions. In recent years, intravascular imaging has become widespread in the evaluation of children with congenital heart defects. A review of the literature on IVUS in endovascular treatment of congenital heart defects is presented and cases of the IVUS use in children with patent ductus arteriosus, descending aortic stenosis after interrupted aortic arch repair and pulmonary stenosis are presented.
REVIEW ARTICLES
What is already known about the subject?
- At menopause, the incidence of osteoporosis and hypertension (HTN) increases sharply due to a decrease in estrogen production.
What might this study add?
- This article details the mechanisms of the relationship between decreased bone mineral density and HTN, which include increased osteoclast activity, sustained increase in parathyroid hormone, angiotensin II and catecholamines, and circadian rhythm disturbances.
- The relationship between HTN and osteopenia depends on the structure and location of the bones.
- Activation of the renin-angiotensin-aldosterone system induces not only HTN, but also osteopenia with microstructural abnormalities reminiscent of osteoporosis.
Hypertension (HTN) and osteoporosis are major age-related conditions, each of which causes significant morbidity and mortality. To date, data have been accumulated on the relationship between hypertension, markers of bone matrix formation and bone resorption. This review article discusses the relationship between hypertension and reduced bone mineral density, as well as previously unknown pathogenetic mechanisms underlying it.
What is already known about the subject?
- Timely care in primary health care reduces the hospitalization risk in patients with ambulatory care sensitive conditions. Taking into account the predictability of most hospitalization cases, it is relevant to search for prevention methods, such as the development and testing of screening tools based on the prognostic effectiveness of hospitalization risk predictors.
What might this study add?
- Evidence on predictors associated with increased hospitalization risk was assessed.
- The conditions under which questionnaires can be used to develop tools in primary health care settings have been identified. The advantages and disadvantages of these methods are revealed.
One of the key tasks facing the medical community and health professionals is the identification of patients at high risk of hospitalization, including emergency one. Currently, various approaches are used to obtain information about certain predictors in a patient that are associated with an increased hospitalization risk, but there is no consensus on which of them are most effective.
Aim. To summarize data from studies that has analyzed the prognostic value of various predictors used in questionnaires or patient surveys associated with an increased hospitalization risk.
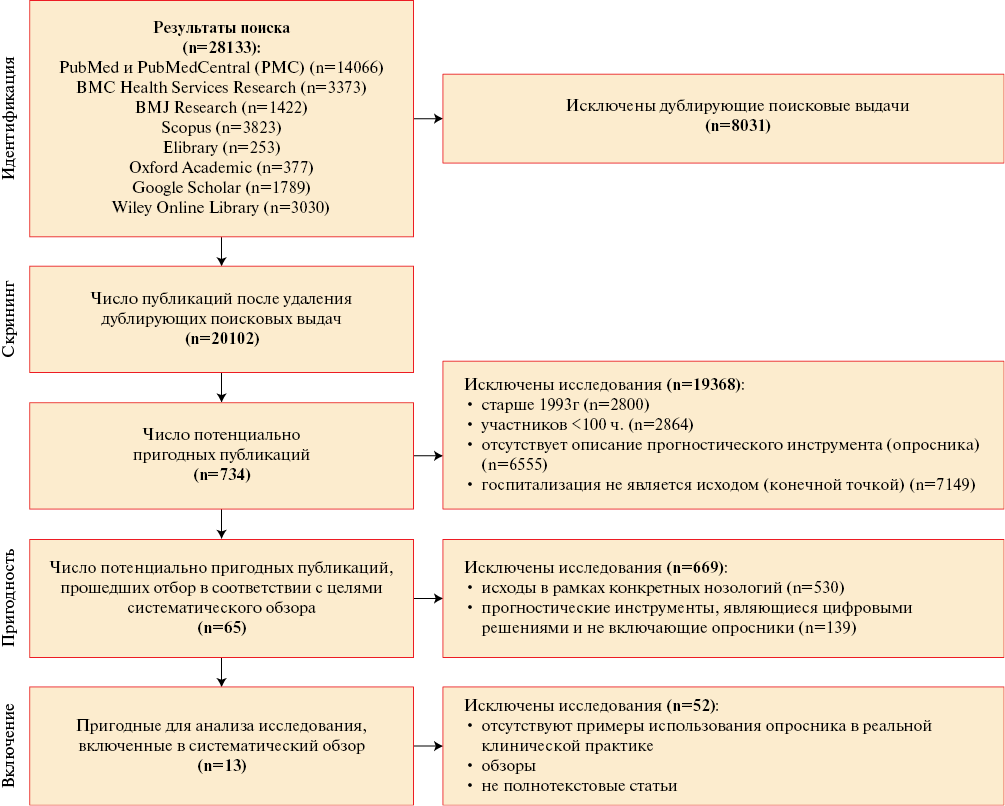
Material and methods. We search for full-text articles in 8 Russian and foreign electronic databases (Scopus, PubMed, BMC Health Services Research, BMJ Research, Google Scholar, e-library, Oxford Academic, Wiley Online Library), published in the period from January 1, 1993 to January 1, 2023 and containing information about questionnaires on hospitalization risk prediction. The study was carried out in 4 following stages: 1 — search for articles using keywords in electronic databases; 2 — duplicate elimination; 3 — search for full-text versions of articles and their assessment for compliance with inclusion/ exclusion criteria; 4 — data analysis, systematization of hospitalization predictors used in questionnaires.
Results. In total, out of 28133 initial publications, 13 full-text papers describing studies that fully met the inclusion/exclusion criteria were admitted to stage 4 and were included in the final analysis. These studies were devoted to the description of 11 questionnaires, their modification or testing. The majority of the articles found (53,8%) were conducted in the United States. When analyzing questionnaires to assess the hospitalization risk, among 61 identified predictors, the following were most often used In questionnaires: "age ≥75 years"; "≥1 hospitalization within one to two years preceding filling out the questionnaire"; "taking ≥5 prescription medications"; "male sex"; "history of diabetes", and "satisfactory/unsatisfactory self-perceived health status". A more detailed analysis of questionnaires to assess the risk of one-year hospitalization among people ≥65 years old found that the following predictors were most often used: "age ≥75 years", "≥1 hospitalization in the period from one to two years before filling out the questionnaire", and "taking ≥3 prescription medications".
Conclusion. Evidence is summarized on predictors used in questionnaires on hospitalization risk assessment. Additional research is needed to validate established predictors in the Russian population, their cause-and-effect relationship, and to search for novel predictors influencing the hospitalization risk among the working age and post-working age population.
ISSN 2619-0125 (Online)