ADDRESS TO THE READERS
ARTERIAL HYPERTENSION
What is already known about the subject?
- Currently, there is significant potential for improving the quality of hypertension control.
- The use of telemedicine technologies can improve the quality of treatment for patients with hypertension.
What might this study add?
- A significant increase in the proportion of patients achieving target BP levels using remote monitoring was demonstrated.
- Remote blood pressure monitoring significantly reduces the risks of cardiovascular events and all-cause death.
- Remote monitoring with automatic data transmission is the most effective.
Aim. To evaluate the efficiency of remote blood pressure (BP) monitoring systems with automatic data transmission in real-world practice.
Material and methods. The study included 12566 patients with both uncontrolled hypertension and those who had achieved target BP levels. Patients underwent remote BP monitoring with an automatic system with data transmission via GSM channel. The analysis included the levels of mean 7-day BP after 4 and 8 weeks of follow-up.
Results. In the total sample of patients, a significant decrease in systolic (SBP) and diastolic BP (DBP) was found after 4 and 8 weeks of monitoring. SBP over 8-week follow-up decreased by -2,5 [-10,0; 4,0] mm Hg, while DBP — by -1,0 [-5,0; 3,0] mm Hg. The number of patients who achieved and/or maintained the target BP level after 8-week follow-up was 8306 (66,1%). Treatment efficacy escape was observed in 1633 (13,3%) patients. Baseline BP levels were not at target in 4692 (38,2%) patients. In this group, a decrease in SBP and DBP was observed over 8 weeks by -9,0 [-17,5; -0,5] and -3,0 [-7,5; 1,0] mm Hg, respectively. Among patients with initially uncontrolled hypertension, 1462 (31,2%) achieved target BP values within 4-week follow-up, while 127 (2,7%) within the next 4 weeks. A significant effect of age on the success of achieving and maintaining target BP levels was revealed. A stable inverse relationship was noted between overweight and obesity and the studied parameter.
Conclusion. Remote BP monitoring using systems with automatic data transmission can significantly increase the proportion of patients achieving and maintaining target BP levels, as well as reduce the risk of cardiovascular events and all-cause death.
What is already known about the subject?
- Inflammatory factors play an important role in the development of hypertension (HTN) and heart failure with preserved ejection fraction. Patients with heart failure with preserved ejection fraction and HTHN with left ventricular hypertrophy are characterized by decreased left atrial strain.
What might this study add?
- In patients with HTN without left ventricular hypertrophy working in the Arctic, initial morphological abnormalities in the form of left atrium strain are determined using the speckle-tracking echocardiography. An inverse correlation was obtained between inflammation factors (cytokines) and early diastolic lateral and septal mitral annular velocities (TDI e'lat and TDI e'sept) in these patients.
Aim. To study the association of left atrial (LA) strain and inflammatory factors in hypertensive (HTN) patients without target organ damage working on a rotational basis in the Arctic.
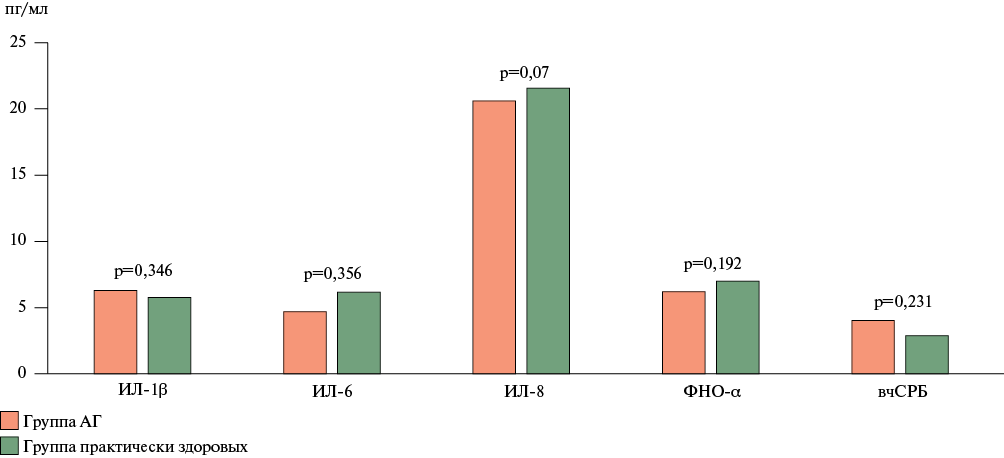
Material and methods. A total of 335 patients were recruited in 20222023 at the Novy Port of OOO Gazpromneft-Yamal, located in the Arctic. The study included 86 patients with HTN and healthy individuals aged 1860 years working by the expeditionary shifts. Inflammatory markers such as interleukin (IL)-1b, IL-6, IL-8, tumor necrosis factor alpha (TNF-a), high-sensitivity C-reactive protein (hsCRP) were determined in the blood serum. We performed transthoracic speckle tracking echocardiography to assess the left atrial reservoir strain (LASr) on the Vivid S70 device, USA, and determination of tissue color Doppler indices.
Results. All patients included in the study were divided into 2 groups: Group 1 — 49 patients with stage 1 hypertension, mainly men (89,8%), middle-aged (45,07±8,1 years), group 2 — 37 practically healthy individuals, the average age was 43,24±7,6 years, men 86,5%. In the group of hypertensive patients, a subgroup of patients with a decrease in LASr compared to the reference index (<39%) and with an increase in LASr (>39%) was identified. There were no patients with LASr ≲23%, which allowed us to rule out heart failure. About half of the patients with HTN had LASr between 23 and 39%. The levels of proinflammatory cytokines (IL-1, IL-6, IL-8) in patients with HTN did not differ from the parameters of healthy individuals. Early diastolic lateral and septal mitral annular velocities (TDI e'lat and TDI e'sept) were significantly lower in the Arctic conditions compared to those in healthy individuals. The correlations between the LA strain and cytokines were studied. An inversely proportional correlation was found between the TDI e'lat and TDI e'sept parameters and the IL-6 level.
Conclusion. Analysis of a subgroup of patients with HTNwithout left ventricular hypertrophy showed an inversely proportional relationship between the cytokine and TDI e'lat and TDI e'sept levels, which suggests an association of inflammatory factors and LA strain in patients with HTN working on a rotational basis in the Arctic.
ACUTE CORONARY SYNDROME
What is already known about the subject?
- High-dose statin monotherapy makes it possible to achieve target values of low-density lipoprotein cholesterol (<1,4 mmol/l) only in 33-42% of patients.
- Coronary vulnerable plaques are a predictor of fatal cardiovascular events.
What might this study add?
- Only 17% of patients after acute coronary syndrome achieved target low-density lipoprotein cholesterol (<1,4 mmol/l) against the background of high-dose statin monotherapy.
- Vulnerable plaques were noted in 44,8% of patients after acute coronary syndrome and were more common in individuals with more severe coronary lesions.
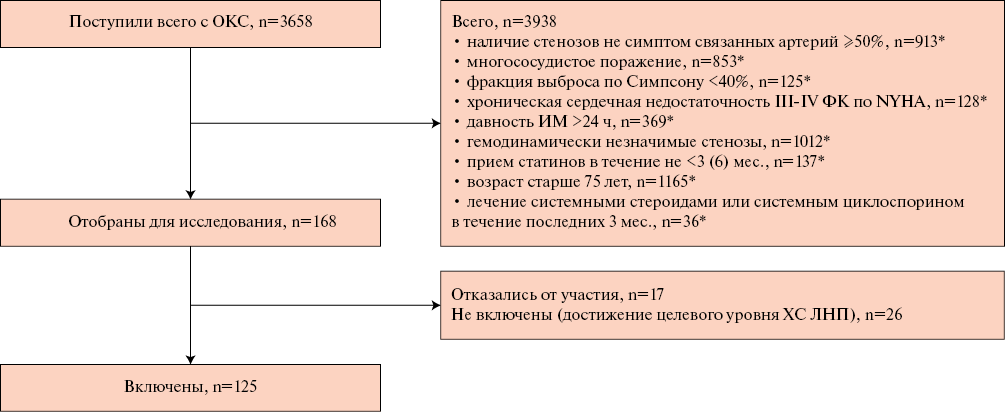
Aim. To assess the detection rate of vulnerable plaques using computed tomography (CT) in patients after acute coronary syndrome (ACS) and percutaneous coronary intervention (PCI).
Material and methods. The study included 125 patients with ACS who underwent PCI (men, 68%; median age, 59 (51-66) years). One month after the index event, patients who did not achieve target low-density lipoprotein cholesterol values were divided into two groups depending on the signs of vulnerable plaques according to CT data.
Results. Vulnerable plaques were detected in 56 (44,8%) patients using CT (69,6% men, median age 60 (51-63) years). Patients with vulnerable plaques were more likely to have right coronary artery (CA) involvement — 53,6 vs 11,6% (p<0,001); left main CA — 33,9 vs 5,8% (p<0,001); left anterior descending artery — 76,8 vs 15,9% (p<0,001); circumflex artery — 48,2 vs 18,8% (p<0,001) compared to patients without vulnerable plaques. The coronary calcium index in patients with vulnerable plaques was significantly higher — 111 (29-247) vs 35 (1-138) (p=0,003). Patients with signs of vulnerable plaques had more severe coronary artery disease according to the segment-stenosis (SSS) and segment-involvement (SIS) scores — 3 (1-4) vs 0 (0-1) (p<0,001) compared to patients without vulnerable plaques.
Conclusion. The detection rate of vulnerable plaques in patients after ACS and PCI not achieved target LDL values while receiving highdose statin therapy was 44,8%. Patients with vulnerable plaques were characterized by more spread atherosclerotic coronary involvement and a high calcium index.
ATRIAL FIBRILLATION
What is already known about the subject?
- The use of oral anticoagulants in geriatric patients may be associated with an increased bleeding risk.
- Cerebral microbleeds (CMBs) can be considered a neuroimaging marker of intracranial hemorrhage.
- The incidence of CMBs in geriatric patients with atrial fibrillation regularly taking direct oral anticoagulants has not been adequately studied.
What might this study add?
- The work is the first observational study to examine the incidence and anatomical location of CMBs in patients with atrial fibrillation aged ≥80 years regularly taking direct oral anticoagulants.
- The high incidence of lobar CMBs at the initial examination and after one year indicates a high risk of intracranial hemorrhage in this cohort of patients.
- The management of geriatric patients requires a multidisciplinary approach with the inclusion of a radiologist to monitor newly detected CMBs and determine their location.
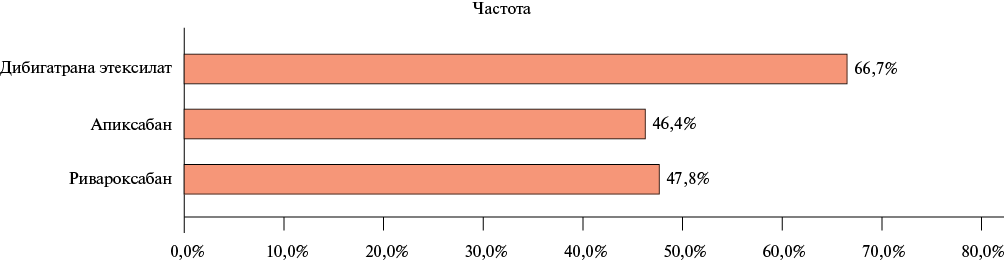
Aim. To study the prevalence and structure of cerebral microbleeds (CMBs) in patients ≥80 years old with non-valvular atrial fibrillation in real-world practice.
Material and methods. Eighty patients were examined (median age 83 (81; 86) years, 72,5% women). All patients underwent brain magnetic resonance imaging using a MAGNETOM Skyra system 3 Tesla (Siemens) during the initial examination and again one year later.
Results. During the initial examination, the detection rate of CMBs was 48,8% and did not differ significantly depending on the direct oral anticoagulant taken (p=0,738). There were 161 CMBs in 39 patients (an average of 4,1±3,6 CMBs per patient). During the repeated examination, newly detected CMBs were in 21,6% of patients. In the initial examination, mixed location of CMBs prevailed (43,6%), mainly in the frontal lobe (25,5%), while in reexamination, lobar location (54,5%) and also mainly in the frontal lobe (43,5%).
Conclusion. The high detection rate of CMBs in patients ≥80 years with non-valvular atrial fibrillation, both at the initial examination and after one year, especially in the lobar location, indicates a high risk of intracranial hemorrhage. Its prevention requires a multidisciplinary approach to the management of such patients.
COVID-19 AND DISEASES OF THE CIRCULATORY SYSTEM
What is already known about the subject?
- E-cigarette (EC) use disrupts the innate immune defense of the lungs, leads to a wide range of pulmonary damages, and is a risk factor for respiratory and many cardiovascular diseases, most often complicating the course of coronavirus disease 2019 (COVID-19).
- The relatively low prevalence and duration of EC use, mainly among the youngest groups of the population, may distort the association of vaping with COVID-19 outcomes.
- Data on the relationship between EC use and COVID-19 incidence and outcomes are scarce and contradictory.
What might this study add?
- The article presents the analysis of national and regional trends, the relationship between EC consumption and COVID-19 outcomes by age and sex groups of the adult population.
- The relationships between the frequency of EC consumption and COVID-19 mortality rates are nonlinear and vary depending on age.
- The obtained offers scope for additional research aimed at an in-depth study of the cause-and-effect relationships between EC consumption and COVID-19 outcomes, taking into account the demographic and socio-economic characteristics of the Russian regions.
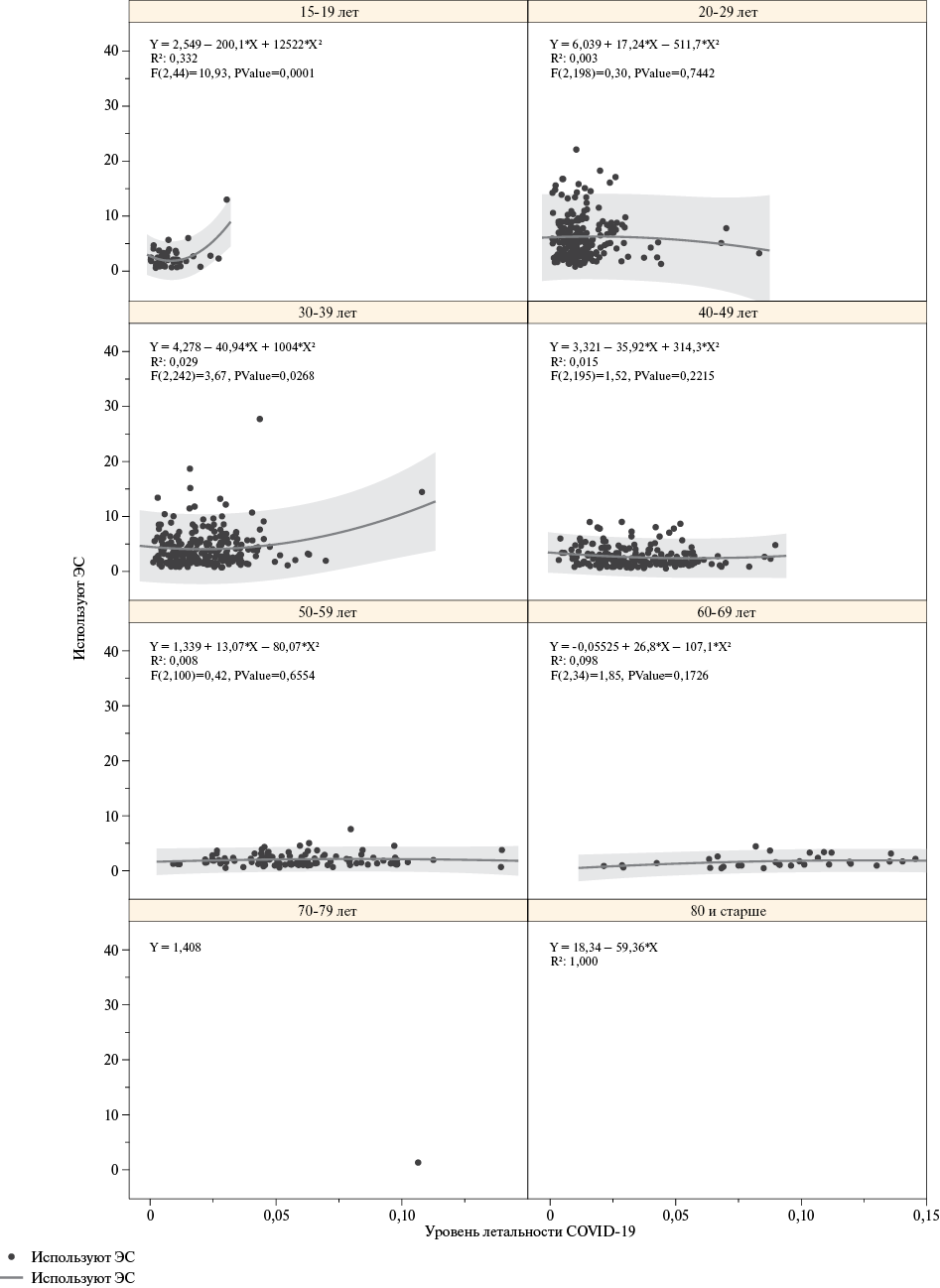
Aim. To study the relationship between hospitalizations, severity and mortality from a coronavirus disease 2019 (COVID-19) with the frequency of e-cigarette (EC) consumption in the Russian Federation for 2020-2021.
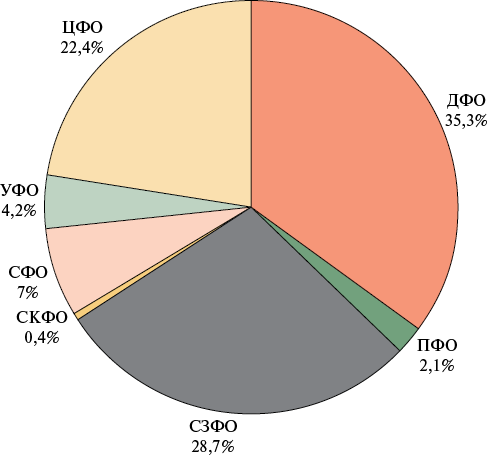
Material and methods. The data on the number of people hospitalized with severe COVID-19 and those who died from COVID-19 for 20202021 in 85 Russian regions from the Federal Registry of COVID-19, as well as data on the status of EC consumption for 2020-2021 in 85 Russian regions from the Rosstat micro-database of the Sample Monitoring of the Population Health were analyzed. An analysis of the relationship between the frequency of EC consumption and the level of hospitalization with COVID-19, COVID-19 severity and mortality by sex and age groups and federal districts (FD) of the Russian Federation was carried out in the quadratic regression model.
Results. Nonlinear relationships between the studied parameters with a characteristic parabolic dependence were obtained. A significant relationship was found between COVID-19 mortality and the frequency of EC consumption in men aged 15-19 years (R2=0,24, p=0,001); in women aged 30-39 years (R2=0,13, p=0,001). The relationships between the level of hospitalizations, severe and fatal outcomes of COVID-19 and EC consumption in most federal districts demonstrate an inverse parabolic relationship.
Conclusion. The relationships between the frequency of EC consumption and COVID-19 indicators are complex and nonlinear. Deep segmented analysis revealed significant associations explaining the contribution of EC consumption to the level of hospitalizations, severe and fatal outcomes of COVID-19 in certain age and sex groups. In the context of the federal districts of the Russian Federation, these relationships are characterized by heterogeneity, apparently due to the impact of a number of demographic and socio-economic factors on COVID-19 outcomes.
What is already known about the subject?
- The coronavirus disease 2019 contributes to the destabilization of blood pressure (BP), the development and progression of dyslipidemia, and worsens the structural and functional arterial characteristics.
- The main goal of treating patients with hypertension and dyslipidemia is to reduce the risk of cardiovascular events, which requires achieving target BP levels and low-density lipoprotein cholesterol.
- Polypill therapy, including antihypertensive and lipid-lowering drugs, helps achieve these goals, improving the cardiovascular prognosis in the long term.
What might this study add?
- A therapeutic strategy described allows achieving not only the optimal level of BP and lipid profile, but also demonstrates a pronounced vasoprotective effect.
- A multifactorial model of the probability of achieving the BP and low-density lipoprotein cholesterol target levels is built, including age, history of hypertension, office systolic blood pressure.
Aim. To identify factors associated with achieving the target blood pressure (BP) and low-density lipoprotein cholesterol (LDL-C) levels with polypill therapy (indapamide, perindopril, rosuvastatin) in patients with hypertension (HTN) and dyslipidemia after a coronavirus disease 2019.
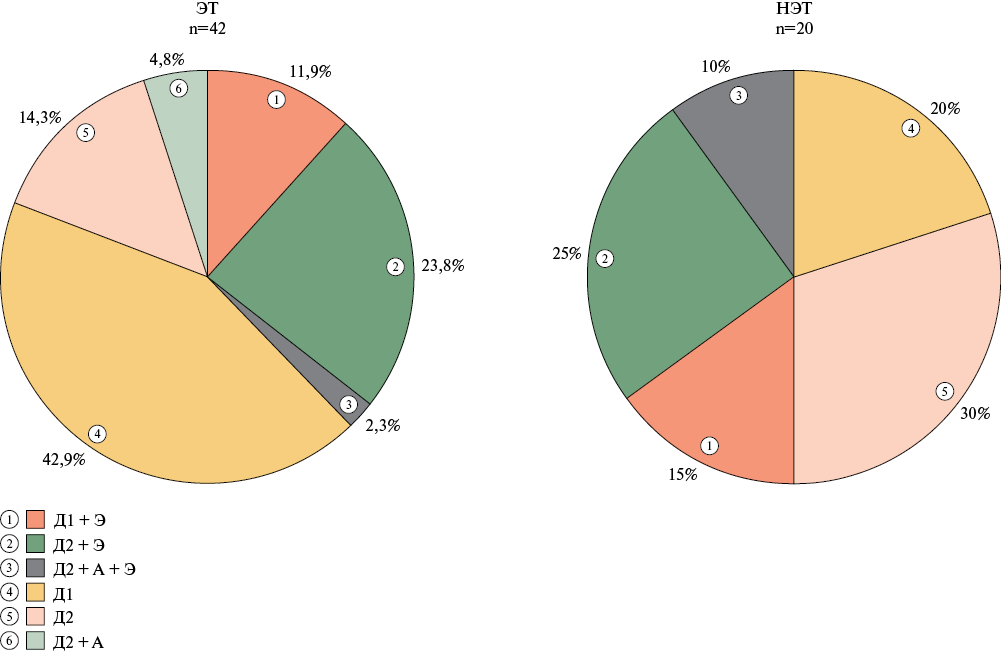
Material and methods. The study included 62 patients who were divided into following groups: 1st (n=42) — BP and LDL-C target levels were achieved after 24 weeks; 2nd (n=20) — target levels were not achieved. Lipid profile, structural and functional characteristics of arteries were determined.
Results. Polypill therapy was characterized by achieving BP and LDL-C target levels in 38,7%, while the addition of amlodipine and ezetimibe increased the effectiveness to 67,7%. In group 1, the carotid intima-media thickness decreased by 11,8%, and in group 2 — by 7% (p<0,05). Only in the 1st group, the proportion of individuals with normal intima-media values increased, the b stiffness index decreased (-15,2%; p<0,01), and the pulse wave velocity decreased according to applanation tonometry. The following predictors of achieving BP and LDL-C target levels with combination therapy, including polypill, were identified: age, history of hypertension, systolic blood pressure, pulse wave velocity, cardio-ankle vascular index.
Conclusion. Simultaneous achievement of BP and LDL-C target levels with polypill therapy in patients with HTN and dyslipidemia after coronavirus infection was accompanied by a pronounced vasoprotective effect. A multifactorial model was created to predict a decrease in BP and LDL-C to target levels, including age, history of HTN, systolic BP.
ФАКТОРЫ РИСКА
What is already known about the subject?
- Smoking is one of the most important modifiable risk factors for cardiovascular and all-cause death risk.
- Smoking cessation helps reduce mortality.
What might this study add?
- According to the 34-year prospective study, smoking significantly increases the cardiovascular and all-cause death risk, especially among younger age groups (20-39 years).
- Smoking cessation was most effective in the younger age group; among the observed older age group, smoking cessation did not affect mortality rates.
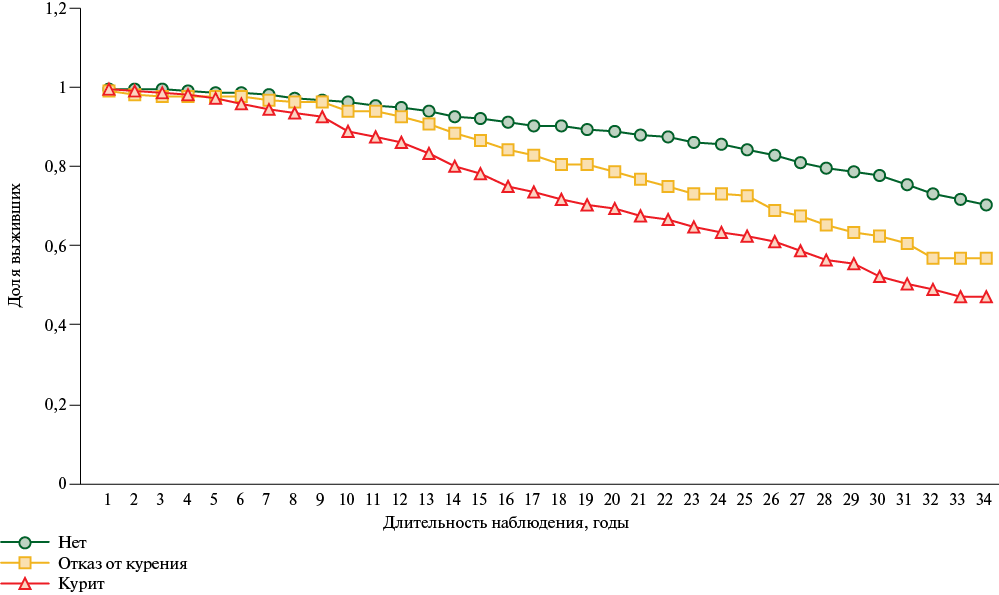
Aim. To study the effect of smoking and smoking cessation on the cardiovascular and all-cause death risk in a long-term 34-year cohort prospective study.
Material and methods. In 1988-1991, 1546 people (630 men and 916 women) aged 20-59 years were examined. Over 34-year follow-up, 556 deaths occurred, including 244 from cardiovascular diseases (CVD).
Results. Tobacco smoking increases the all-cause death risk by 2,4 times, and among people aged 20-39 by 3,5 times. Among men who quit smoking, the death risk is 1,9 times higher compared to nonsmokers. Among older people, quitting smoking did not affect the death risk. Smoking increases the cardiovascular death risk by 1,9 times, and among people under 40 by 3,6 times. Among those who quit smoking, the cardiovascular death is 1,7 times higher compared to non-smokers. The 34-year survival rate among non-smokers is 70,2%, smokers — 47,2%, and those who quit smoking — 57,1%.
Conclusion. A significant contribution of smoking to the increased cardiovascular and all-cause death risk was revealed. Smoking cessation in the older age group is accompanied by a persistent increased cardiovascular and all-cause death risk. The best age to quit smoking is before 40 years.
What is already known about the subject?
- Preventive counseling is an effective intervention for secondary prevention of chronic non-communicable diseases, incl. complications of ischemic heart disease, by correcting the risk factors included in the adult population medical examination program.
What might this study add?
- For the first time, the coverage of preventive counseling of patients on the main cardiovascular risk factors after myocardial infarction was studied in 13 Russian regions. An assessment of the completeness of coverage of preventive counseling among patients after myocardial infarction and the identification of factors associated with increased consultative activity will allow developing the approaches to improving medical follow-up.
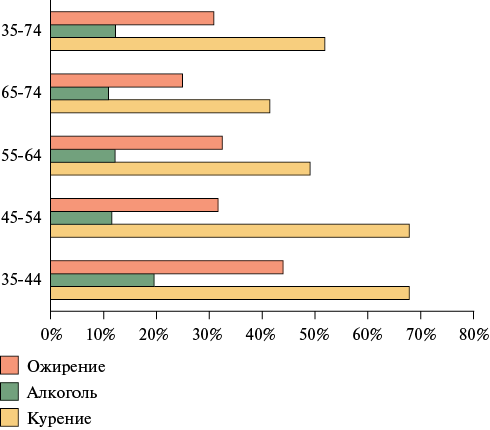
Aim. To assess the coverage of preventive counseling on the main modifiable cardiovascular risk factors (RFs) in patients after myocardial infarction (MI) and to identify factors associated with increased counseling activity within a year after the coronary event.
Material and methods. The study included 1107 patients with MI aged 35-75 years using a special randomization approach. After 6 months, 889 people were interviewed, and after 12 months — 703 people. At the hospital stage, the smoking status and alcohol consumption were clarified using the Cut down, Annoyed, Guilty, Eye-opener (CAGE) questionnaire. After 6 and 12 months, we clarified whether preventive counseling on the main cardiovascular RFs had been carried out. Social status, changes in life history and disease were also clarified to identify factors associated with receiving preventive counseling.
Results. Six and twelve months after MI, preventive counseling on smoking cessation was carried out in 63,8 and 58,4% of smoking patients, respectively; on alcohol cessation — in 16,5 and 14,9%. Patients with obesity (odds ratio (OR) 0,7; confidence interval (CI): 0,48-1,0; p=0,053) and type 2 diabetes (OR 0,49; CI: 0,29-0,82; p=0,008) received counseling on smoking cessation significantly less frequently. Smoking patients (OR 2,87; CI: 1,79-4,66; p<0,001) and those with left ventricular ejection fraction <50% (OR 1,6; CI: 1,01-2,56; p=0,048) received counseling on alcohol cessation more frequently. After 6 and 12 months, 71,5 and 71,6% of patients were consulted on dietary issues, while 56,8 and 31,6% of patients on physical activity, respectively. On dietary issues, obese patients received consultations significantly more often (OR 1,51; CI: 1,02-2,25; p=0,04). Patients observed by a cardiologist more often received consultations on healthy eating (OR 2,1; CI: 1,423,12; p<0,001) and physical activity (OR 2,0; CI: 1,35-2,97; p<0,001).
Conclusion. The study results revealed a deficit in preventive counseling on the main modifiable cardiovascular risk factors and their complications.
РREVENTION OF CARDIOVASCULAR DISEASES
What is already known about the subject?
- Technological progress in the early 21stcentury has led to an enhancement of medicine capabilities, making it possible curing previously fatal diseases and preclinical diagnosing many chronic diseases.
- Increasing life expectancy and reducing mortality depend not only on primary prevention, but also on the organization of effective secondary prevention of noncommunicable diseases.
What might this study add?
- Among the causes of hospitalization, cardiovascular diseases occupy the main place, which requires improving medical examination and outpatient care among people at high cardiovascular risk.
- Among the priorities of secondary prevention of noncommunicable diseases, an important place is occupied by improving educational work to increase patient adherence to drug correction and achieving target levels of major risk factors.
- Optimization of material and technical support, as well as improving the staffing of doctors and nursing staff are an important link in the organization of secondary prevention in primary health care.
Aim. To determining the potential of secondary prevention of noncommunicable diseases (NCDs) at the outpatient and inpatient stages by conducting a cross-sectional medical and social survey of a cohort of physicians from various Russian cities.
Material and methods. Physicians from outpatient clinics (16 cities, 545 physicians) and hospitals (13 cities, 151 physicians) took part in the cross-sectional study. The survey was carried out using an original questionnaire, in the development of which experts from the National Medical Research Center for Therapy and Preventive Medicine and public health professionals took part. The questionnaire consisted of 9 questions, including sex and age characteristics, frequency of various nosological units, medication adherence, subsidized drug provision, interaction with outpatient doctors, and staffing of doctors and midlevel personnel. Answers were offered for each question in several gradations. Depending on the population size, the cities were divided into 4 following subgroups: population >2 million people, 1-2 million people, 0,4-1 million people and <400 thousand people.
Results. According to the obtained results, in outpatients clinics and hospitals, coronary artery disease ranks first in terms of the frequency of adult population visits and accounts for ~40% of NCDs. Patients with a diagnosis of heart failure are 1,4 times more likely to visit hospitals compared to outpatient clinics. The frequency of detection of other chronic diseases in outpatient clinics and hospitals has a similar picture and in total amounts to 50% of visits for NCDs. Among hospitalized patients, persons of both sexes aged 65 years dominate, while at the outpatient level it is <2 times. Patients aged 60-64 years, regardless of sex, equally often seek outpatient and inpatient care. Subsidized provision of essential drugs in every second case is provided at a satisfactory level (50-75%). A comparable number of patients receive drugs up to 50% of cases. Every second patient is not adherent to drug and non-drug therapy to varying degrees, and the opinion of outand inpatient physicians is comparable. It should be noted that in outpatient clinics, the understaffing of doctors and paramedical personnel reaches 50%.
Conclusion. Given the dominant position of cardiovascular diseases among the causes of hospitalization and outpatient care due to older age groups, outpatient follow-up and care among high-risk individuals should be improved. Among the priorities of secondary prevention of NCDs, an important place is occupied by improving educational work to increase patient adherence to drug correction and achieving target levels of the main risk factors. Optimization of material and technical support, including drug provision of health facilities, as well as improving the staffing of doctors and nursing staff play a key role in managing secondary prevention in primary health care.
INTERDISCIPLINARY PROBLEMS IN CARDIOLOGY
What is already known about the subject?
- Postoperative pneumonia (PP) is a common complication of cardiac surgery, negatively affecting clinical outcomes and economic aspects of treatment.
- Known risk factors include old age, chronic diseases, prolonged ventilation, and complexity of the surgery.
What might this study add?
- The prevalence and key predictors of pneumonia after coronary artery bypass grafting were determined as follows: preoperative white blood cell count, aortic cross-clamp time, and maximum postoperative creatine phosphokinase level.
- It was found that combined surgeries do not increase the PP risk compared to isolated coronary artery bypass grafting.
- Sex was not associated with the PP risk.
Aim. To assess the prevalence and predictors of postoperative pneumonia (PP) after coronary artery bypass grafting (CABG) based on inhospital registry data.
Material and methods. This retrospective study of 925 patients who underwent elective CABG in 2017-2019 based on inhospital registry data. Combined intervention was performed in 11% of cases. PP was diagnosed according to national guidelines. Multivariate logistic regression was used to identify predictors. Preoperative, surgical, and postoperative variables were included in the association analysis.
Results. The incidence of PP was 8,7%. PP developed on day 5,5 [3; 8] (Me [Q25; Q75]) after CABG. Sex did not affect the risk. In univariate analysis, significant factors for PP were preoperative white blood cell (WBC) count, aortic cross-clamp time (ACCT), and maximum postoperative creatine phosphokinase (CPK) level. In the multivariate model, the independent nature of predictors was confirmed: preoperative leukocyte count (OR — odds ratio (odds ratio) =1,11; p=0,008), AC duration (OR=1,07; p=0,045), and postoperative CPK level (OR=1,04; p=0,018). Combined surgeries did not increase the risk.
Conclusion. PP is a serious complication of cardiac surgery, negatively affecting clinical outcomes and economic aspects of treatment. After CABG, PP was detected in 8,7% of cases in the examined cohort. There were following key predictors: preoperative WBC count, ACCT, and maximum postoperative CPK level. The obtained results indicate the possible benefit of monitoring individual inflammatory markers and minimizing ACCT for predicting and reducing the risk of pneumonia.
What is already known about the subject?
- It is known that patients undergoing coronary artery bypass grafting require antiplatelet therapy; the standard is acetylsalicylic acid. There are attempts to prescribe dual antiplatelet therapy in patients with stable coronary artery disease undergoing coronary artery bypass grafting. However, to date, the benefit-risk ratio of such treatment is unclear, and the optimal candidate for dual antiplatelet therapy has not been determined.
What might this study add?
- Addition of clopidogrel to aspirin helps to ensure better patency of small (<1,5 mm) diameter bypass grafts in diffuse coronary artery disease.
Aim. To study the clinical outcomes and the frequency of bypass graft occlusions in patients with diffuse coronary artery disease (CAD) and small (<1,5 mm) diameter of bypassed coronary arteries (CA) one year after coronary artery bypass grafting (CABG) while taking various antithrombotic therapies (ATT) (aspirin and a combination of aspirin with clopidogrel).
Material and methods. This prospective randomized study included 94 patients with a stable diffuse multivessel CAD with a small (<1,5 mm) vessel diameter, who underwent uncomplicated CABG. The patients were randomized into 2 following groups: acetylsalicylic acid (ASA) monotherapy (n=41) and ASA+clopidogrel therapy (n=53). The median follow-up (interquartile range) was 20 (12; 24 months). All participants underwent computed tomographic (CT) bypass angiography.
Results. There were a total of 349 bypasses with a total occlusion rate of 54 (16%). The bypass occlusion rate in the ASA and ASA+clopidogrel groups was very close as follows: 19 vs 13% (p=0,191). In the subanalysis of the bypass graft function related to arteries with a diameter <1,5 mm, occlusions developed more often in the ASA group (39 vs 12%, p=0,005). This difference was formed due to the gap between the groups in the bypass graft occlusion rate related arteries of the smallest diameter (≲1 mm) (60 vs 17%, p=0,006). The angina recurrence rate with aspirin monotherapy was slightly higher than with "enhanced" ATT (20 vs 13%, p=0,480).
Conclusion. Bypass graft occlusions related to arteries of small (<1,5 mm) diameter, assessed one year after CABG, develop significantly less often with ASA+clopidogrel combination therapy.
LITERATURE REVIEW
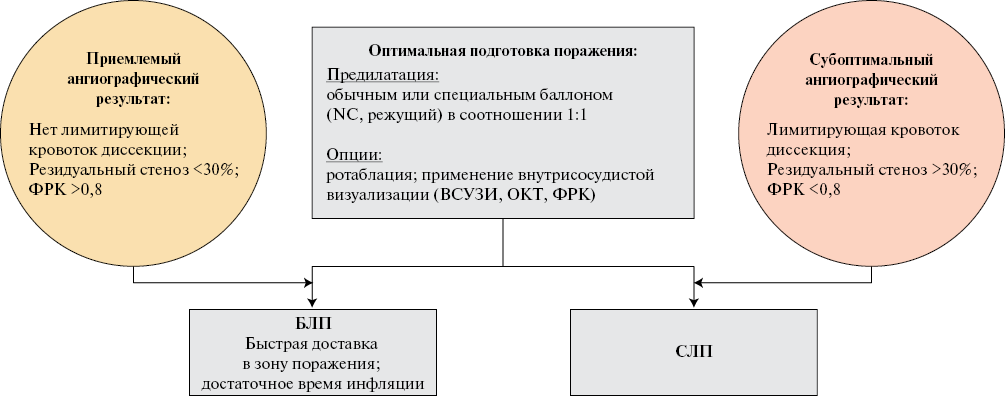
What is already known about the subject?
- Coronary balloon angioplasty and stenting is the standard of surgical treatment for coronary artery disease.
- The use of a metal stent is associated with local hemodynamic impairment and chronic inflammation, leading to restenosis.
What might this study add?
- The use of a drug-eluting balloon (DEB) eliminates the disadvantages of metal stents and can become an effective and safe alternative to coronary stenting.
- The review presents an analysis of the latest publications demonstrating the safety and effectiveness of DEB in the treatment of de novo coronary lesions in a number of clinical situations.
In the last decade, the disadvantages of coronary artery (CA) drugeluting stenting have become increasingly obvious. Metallization of the artery, loss of vasoreactivity and chronic inflammation at the implantation site lead to restenosis and an increased risk of repeated revascularization. In this regard, the "leaving nothing behind" concept is attracting increasing interest, which came to coronary revascularization from lower limb arterial disease strategies. The treatment methods within this concept in CA include the use of biodegradable scaffolds and drug-eluting balloons (DEB). Despite the fact that both Russian and foreign guidelines for DEB establish the role of in-stent restenosis treatment, large studies demonstrate the efficacy and safety of DEB in the treatment of de novo coronary lesions. The review systematizes the latest data on the DEB potential in the treatment of de novo native coronary lesions.
ISSN 2619-0125 (Online)