ADDRESS TO THE READERS
HEART RATE VARIABILITY
What is already known about the subject?
- The predominance of autonomous regulation is associated with better adaptation to academic load and stress, while the predominance of central regulation may indicate increased stress in the regulatory systems.
What might this study add?
- The influence of the type of autonomic regulation on myocardial functional state and the central nervous system has been established.
- In students with a pronounced dominance of autonomous and central heart rhythm regulation, a deterioration in the myocardial functional state and central nervous system and a decrease in mental performance were revealed.
Aim. Rationale of the individual typological approach in the analysis of the body function of medical students.
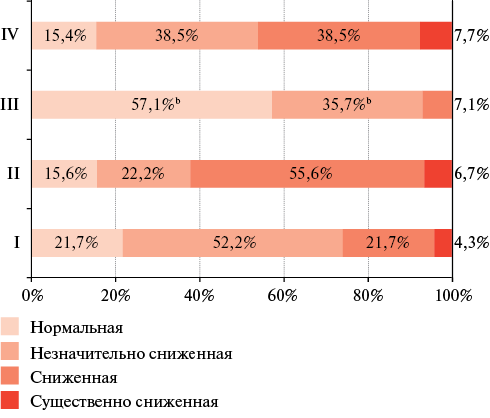
Material and methods. In students with moderate (Group I) and high (II Group) dominance of central regulation, with moderate (III Group) and high (IV Group) predominance of autonomous regulation, a comparative analysis of heart rate variability parameters, the functional state of the myocardium and the central nervous system was carried out.
Results. We found that 53,3% of group III students had no deviations in myocardial function. There were the maximum values of nervous response stability (2,0 [1,5-2,3] units) and functional capability of the nervous system (3,3, [2,7-3,5] units) relative to students of other groups, as well as the formation of normal and slightly reduced mental performance (93,6%), satisfactory biological adaptation (33,3%). In group II students, relative to group III students, there were an increase in the "myocardium" index by 1,2 times, "rhythm" index by 1,8-1,9 times, T wave alternans by 1,3 times and myocardial electrical instability by 2 times, as well as a decrease in nervous system stability by 2,5 times, its functionality by 1,7 times, the formation of reduced performance (55,6%) and unsatisfactory biological adaptation (35,2%). In group IV students, the functional state was characterized by heart rhythm dysregulation (94,1%), borderline myocardial function deviations (76,5%), and a 1,7-fold decrease in nervous reaction stability and 1,3-fold decrease functional capability of the nervous system relative to group III students, reduced performance (38,5%) and unsatisfactory biological adaptation (58,8%).
Conclusion. Differentiation of students depending on the individual typological characteristics of the autonomic heart rate regulation makes it possible to identify students at risk with a pronounced dominance of autonomous and central heart rate regulation, which becomes the starting point for the implementation of differentiated methods of wellness education.
ISCHEMIC STROKE
What is already known about the subject?
- Hypertension is one of the most important risk factors for ischemic stroke.
What might this study add?
- Systolic and pulse blood pressure indices within the month before stroke and their changes during the acute ischemic stroke help to predict stroke severity and functional outcome.
- Blood pressure monitoring at days 1-2 and 9-10 after stroke helps to identify patients with increased BP variability, which is important to consider when administering antihypertensive therapy.
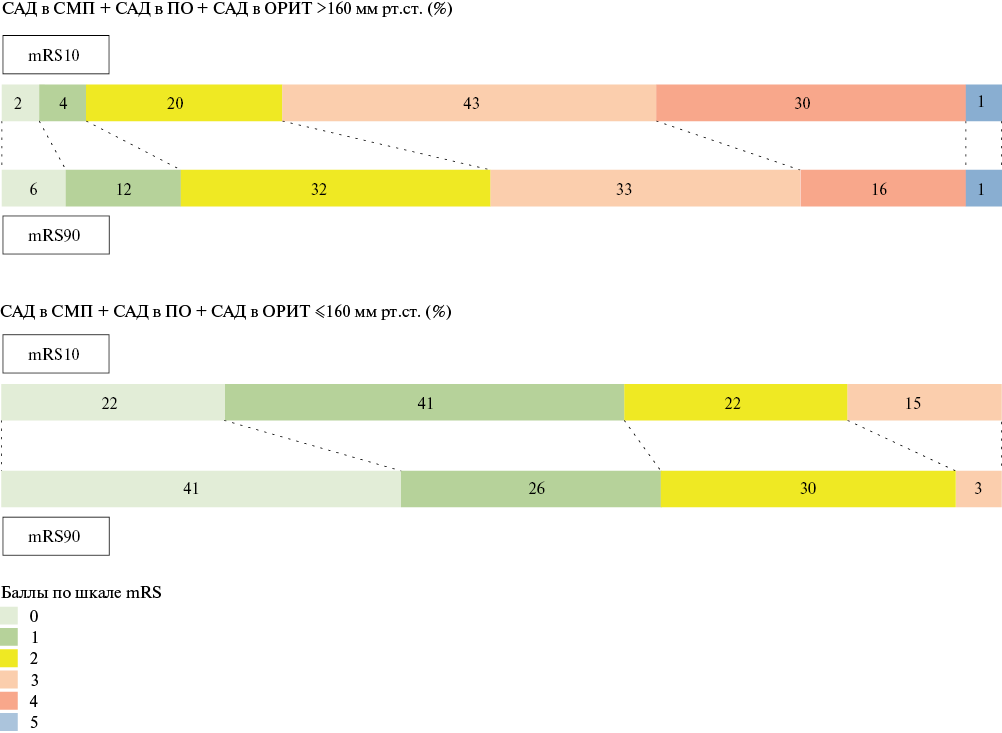
Aim. To study changes in blood pressure (BP) in patients with acute hemispheric ischemic stroke (AIS), to correlate BP in patients with AIS with BP in patients with chronic brain ischemia, and to study the association of various BP indices with stroke severity and recovery.
Material and methods. We included 235 patients with hemispheric AIS (age 64±11 years; women, 41,3%). BP was assessed 6 times as follows: by patient’s self-measurement during the month before the stroke onset, in the ambulance, in the admission department, in the intensive care unit using 24-hour blood pressure monitoring (BPM), in the neurologic department (BPM), and 90 days after stroke. In patients with chronic cerebral ischemia (178 patients, age 62±13 years, 46,1% women), BP was assessed 3 times: by patient’s self-measurement during the month before hospitalization, in the admission department, and in the neurologic department (BPM).
Results. Patients with AIS within the month before stroke had higher systolic and pulse pressure than patients with chronic cerebral ischemia. During the acute stroke period, patients with AIS despite reaching target systolic and diastolic BP had significantly increased variability of systolic and diastolic BP compared to patients with chronic brain ischemia. Systolic BP ≥160 mm Hg recorded consecutively in ambulance, in admission department, and in intensive care unit, as well as pulse pressure ≥60 mm Hg, and systolic BP variability ≥18 mm Hg recorded on day 1-2 and day 9-10, positively correlated with National Institute of Health Stroke Scale (NIHSS) score (r≥0,37, p≤0,0017) on day 10 and with modified Rankin Scale (mRS) score (r≥0,29, p≤0,006) on day 90.
Conclusion. Patients with hemispheric AIS had significantly higher systolic BP and pulse pressure within the month before stroke. During the first 10 days of AIS persistent increase in systolic, diastolic, and pulse pressure, and BP variability was associated with more severe stroke and less favorable outcome. These results should be taken into account when administering antihypertensive treatment.
STRESS IN THE POPULATION
What is already known about the subject?
- Psychological stress, depression can induce a sensitization effect with increased inflammatory responses to stressors and can act as a maladaptive response.
- In young adults, population-based assessment of proinflammatory cytokines such as interleukin-6 (IL-6), which play an important role in psychological stress and depression and may mediate their psychological, behavioral and neurobiological manifestations, is essential.
What might this study add?
- Median levels of IL-6 are higher in with high depression levels than without it, and in the presence of job stress than in the absence of it.
- Differences in mean plasma IL-6 levels were even more pronounced among individuals with combined work stress and high levels of depression than with depression or work stress separately.
Aim. To study the association of interleukin-6 (IL-6) levels with depression and stress at work among young people (25-44 years old) in Novosibirsk.
Material and methods. A random representative sample of young people (25-44 years old) in Novosibirsk was surveyed (975 people of both sexes; response rate, 71%) in 2013-2016 on the basis of Research Institute of Internal and Preventive Medicine — branch of the Institute of Cytology and Genetics (FWNR-2024-0002). All respondents signed informed consent. The World Health Organization MONICA-Psychosocial (MOPSY) scale was used to assess depression. Work-related stress was determined using the Karasek’s scale included in the program protocol. Quantitative determination of IL-6 was carried out in the laboratory of clinical biochemical and hormonal studies of therapeutic diseases of the Research Institute of Internal and Preventive Medicine — branch of the Institute of Cytology and Genetics.
Results. High level of depression among people of both sexes aged 25-44 years were 11,9% (among men — 8,5%, among women — 14,6%). The level of IL-6 was higher in individuals of both sexes with high level of depression — 1,33 [0,72;3,92] pg/ml than without depression — 1,16 [0,63;2,37] pg/ml) (p=0,002). In women with high level of depression, IL-6 value was higher (1,31 [0,72;3,86] pg/ml) than in those without depression (1 [0,53;2,03] pg/ml) or a moderate depression — 1,06 [0,58;2,14] pg/ml, (p=0,002). The level of IL-6 was higher among people of both sexes who had changed occupation within the last 12 months (1,4 [0,67;3,58] pg/ml) than among those who had no changes — 1,12 [0,63;2,04] pg/ml. Among participants who assessed their work responsibility as very high, the median levels of serum IL-6 were higher (1,7 [0,72;5,48] pg/ml), than among people with high work load (1,37 [0,58;5,18] pg/ml), as well as with a moderate (1,21 [0,63;2,5] pg/ml) and a slight (1,09 [0,63;1,98] pg/ml) work load.
Conclusion. A significantly higher level of IL-6 was found in depression and workplace stress among young people (25-44 years old) compared to people without depression and not experiencing workplace stress.
HEART FAILURE
What is already known about the subject?
- Heart failure with preserved ejection fraction (HFpEF) is a heterogeneous phenotype of chronic HF characterized by comorbidity.
- The central theory of the development and progression of HFpEF is considered to be inflammatory.
What might this study add?
- Factors associated with an unfavorable course of HFpEF during a one-year prospective follow-up in conditions of chronic low-intensity inflammation are presented.
Aim. To analyze the prognostic significance of clinical, anamnestic and paraclinical parameters in patients with heart failure with preserved ejection fraction (HFpEF) and non-obstructive coronary artery disease.
Material and methods. The study included 54 patients. Cardiac and lung ultrasound was performed. In addition, the level of N-terminal pro-brain natriuretic peptide (NT-proBNP), interleukin-1β, interleukin-18, growth differentiation factor 15 (GDF-15), and cryopyrin was determined. The level of quality of life, anxiety and depression, and adherence to treatment were analyzed.
Results. The patients were divided into 2 following groups: group 1 (n=22) with an unfavorable course and group 2 (n=32) with a favorable disease course. Basic echocardiographic parameters, as well as the number of B-lines in lungs, were comparable in both groups. An unfavorable HFpEF course was associated with a longer history of hypertension — 17,5 [10;20] and 7 [5;15] years (p=0,03), smoking — 36,4 and 9,4% (p=0,035), impaired carbohydrate metabolism — 54,5 and 15,6% (p=0,003) and lower adherence to treatment (p=0,02). In group 1, GDF-15 levels were higher than in group 2 — 1841 [1237;3552] vs 1709,5 [1158;2492] pg/ml (p=0,026).
Conclusion. Low-intensity subclinical inflammation, the predisposing factors of which are smoking, impaired carbohydrate metabolism, and a long history of hypertension, is associated with higher GDF-15 values in patients with HFpEF and, along with low patient adherence to treatment, has an adverse effect on the clinical course of heart failure.
RESEARCH METHODS
What is already known about the subject?
- Electrocardiography recording identifies patients with a long QT interval at high risk for fatal arrhythmias.
- An integrated approach to the diagnosis of cardiovascular toxicity allows early verification of cardiovascular complications.
- Analysis of left ventricular ejection fraction as part of the diagnosis of cardiovascular complications remains a relevant fundamental method.
What might this study add?
- Variability in clinical phenotypes of cardiovascular toxicity dictates the need to reconsider the criteria for adverse cardiovascular events.
- Dynamic monitoring of left ventricular longitudinal strain can be considered the most promising direction in relation to identifying subclinical myocardial dysfunction.
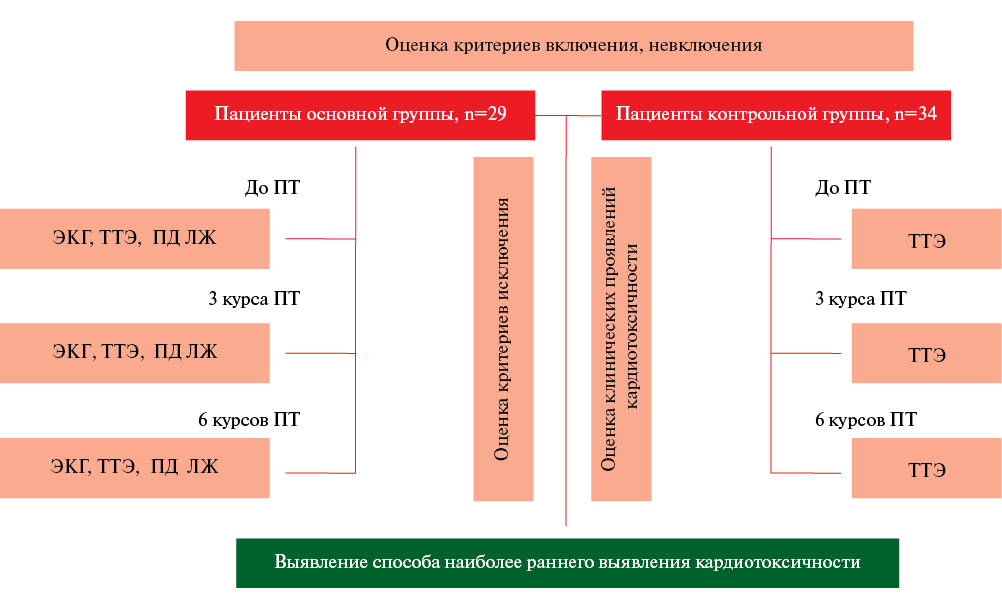
Aim. To study the possibilities of instrumental research methods in relation to the earliest detection of cardiovascular events in oncohematological patients receiving antitumor immunochemotherapy, as well as to determine the requirements for documenting adverse events.
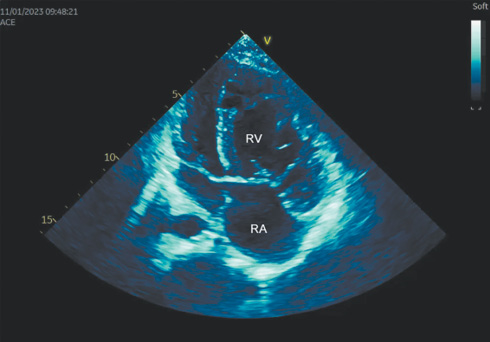
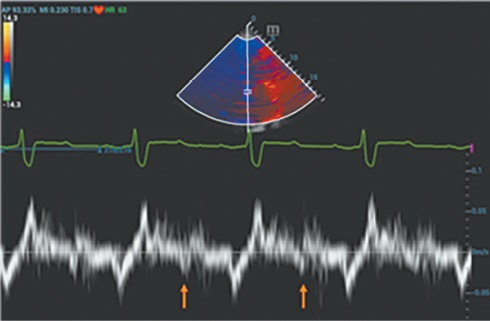
Material and methods. For the study, 63 patients were prospectively selected with a diagnosis of indolent non-Hodgkin lymphoma, who were indicated for antitumor immunochemotherapy. The patients were examined in three stages (before treatment, after 3 and 6 cycles of therapy) and divided into 2 groups by simple randomization. Cardiovascular toxicity in the main group of patients was assessed using 3D transthoracic echocardiography, analysis of left ventricular (LV) global longitudinal systolic strain and electrocardiography. The control group underwent a standard 3D echocardiography with analysis of LV ejection fraction. Clinical manifestations of cardiovascular events were assessed in all patients during treatment.
Results. According to the study, significant changes were obtained in LV ejection fraction on the third visit — a decrease from 58,9±1,07 to 48,1±0,73% (p<0,05) and from 57,7±1,13 to 49,4±0,58% (p<0,05) in patients of the main and control groups and global longitudinal LV strain from |21,1±1,18 to |14,0±1,61 |% (p<0,05) in patients of the main group. A mixed clinical phenotype of cardiovascular toxicity was the most common among all patients. An integrated approach to the early diagnosis of cardiovascular events makes it possible to identify a larger percentage of patients with subclinical myocardial dysfunction.
Conclusion. The long period of latent cardiovascular toxicity emphasizes the need for early verification of cardiovascular complications of antitumor therapy and expansion of the established paraclinical diagnostic minimum. In addition, taking into account the accumulated experience, recommendations are presented for the preparation of medical documentation in order to ensure the safety and quality of care.
CLINICAL CASES
- Congenital extrahepatic portocaval shunt (CEPS) is a rare and generally unrecognized cause of severe pulmonary arterial hypertension (PAH) that should be excluded in all cases of unexplained PAH.
- Timely diagnosis and surgical treatment of portal system anomalies could prevent multisystem involvement, including PAH.
- Late (after 2 years of life) surgical correction could potentially reduce the severity of hemodynamic disturbances.
- Any elective surgical intervention in patients with high-risk PAH should be carried out with calculation of perioperative risk and only after achieving target hemodynamic parameters with targeted PAH therapy.
The article provides a case of pulmonary arterial hypertension (PAH) associated with congenital extrahepatic portocaval shunt (CEPS), or Abernethy malformation, in a 17-year-old female patient. CEPS, which remained undiagnosed for a long time, manifested with severe encephalopathy at an early age. By the age of 6 years, it was complicated by PAH, and by the age of 9 years — by hepatic focal nodular hyperplasia. In the absence of timely surgical treatment and adequate therapy of CEPS, PAH progressed. Combined dual therapy for PAH, prescribed only at age 14, was ineffective. Despite the potential for clinical and functional improvement documented with combination triple therapy at 17 years of age, the patient continued to meet criteria for a high risk of adverse events, including mortality. Two months after the initiation of triple therapy for PAH, not achieving the target hemodynamic characteristics that would reduce operative and perioperative risks lead to an attempt of surgical treatment of CEPS, which led to the patient death in the early postoperative period. The description of this case report shows the difficulties of diagnosing a rare form of portopulmonary hypertension, the modern possibilities of drug therapy for a severe, potentially curable PAH in the early stages.
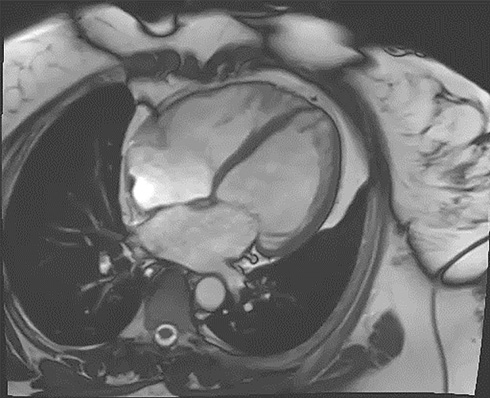
- A patient with left ventricular hypertrophy underwent cardiac gadolinium-based contrast-enhanced magnetic resonance imaging to clarify the disease origin.
- According to magnetic resonance imaging, a subendocardial pattern of myocardial contrast accumulation, atypical for hypertrophic cardiomyopathy, was revealed, which complicated further differential diagnostic search.
Left ventricular (LV) hypertrophy implies structural cardiac changes and, as a consequence, an increase in myocardial mass. Currently, there are many causes of this condition as follows: hypertension, aortic stenosis, hypertrophic cardiomyopathy, exercise, storage diseases (AL, ATTR amyloidosis, Danon disease, Anderson-Fabry disease, etc.), metabolic disorders. Despite the currently existing diagnostic algorithms for LV hypertrophy, establishing a correct diagnosis can take a long time, and controversial research results can lead to false conclusions. This article presents a case report of a patient with LV hypertrophy, an atypical clinical performance and ambiguous paraclinical data, which led to certain diagnostic difficulties.
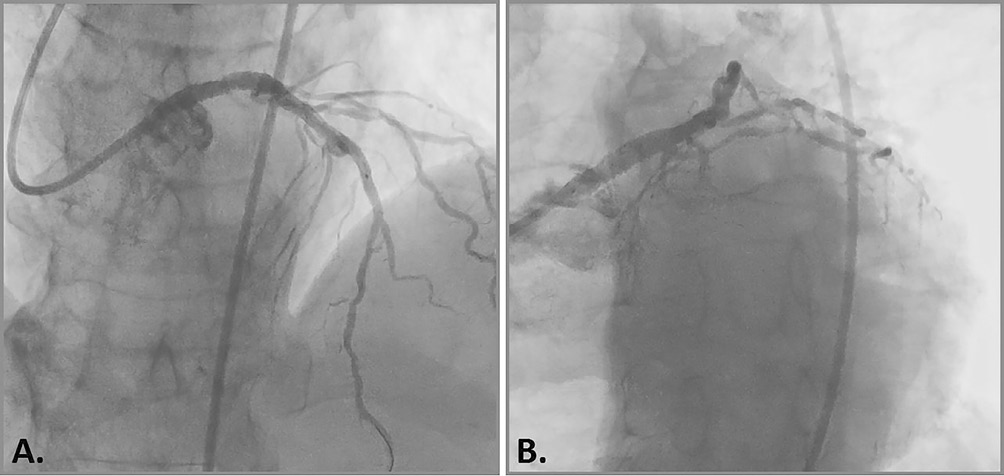
- Coronary calcification is a high-risk factor for periprocedural complications.
- Rotational atherectomy to modify the atherosclerotic plaque and prepare the calcified portion of the artery for stenting makes it possible to for optimal stent implantation.
- Intravascular imaging techniques makes it possible to minimize the risks of periprocedural complications and improve the long-term prognosis of stent patency.
The revascularization strategy for severe calcification is one of the most pressing problems of modern percutaneous coronary interventions, since it is observed more and more often and significantly complicates traditional endovascular treatment. Currently, the method of choice for severe coronary calcification is rotational atherectomy, which allows modification of atheromatous mass with an increase in the vessel lumen to allow satisfactory balloon angioplasty and stenting. This article presents a case of a patient at very high cardiovascular risk with a burdened coronary history and severe clinical symptoms of exertional angina while receiving the optimal multiagent therapy. The examination revealed a multivessel coronary calcification, but the patient was denied coronary artery bypass grafting due to high perioperative risks. SYNTAX (Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery score) score I – 25,5 points, SYNTAX score II — 40,4% and 70,1% for percutaneous coronary intervention and coronary bypass surgery, respectively, European System for Cardiac Operative Risk Evaluation (EuroSCORE II) — 4,95%. Attempts at traditional percutaneous intervention were unsuccessful and the patient underwent endovascular rotational atherectomy followed by stenting of affected coronary segments, against the background of which there was an improvement in exercise tolerance with a decrease in angina class.
- One of the rare phenotypes of left ventricular noncompaction is a combination with an atrial septal defect.
- Cardiac arrhythmias in such patients pose a risk of thromboembolism and sudden cardiac death, and also contribute to heart failure progression.
- If antiarrhythmic therapy is ineffective, pulmonary vein cryoballoon ablation is indicated to eliminate the source of atrial fibrillation. If ventricular ectopic activity persists, the anticonvulsant drug carbamazepine can be used.
Introduction. Left ventricular noncompaction (LVNC) is a rare heterogeneous pathology characterized by a two-layered structure with a predominance of non-compact layer in the form of multiple trabeculations and pockets between them, communicating with the left ventricular cavity. One of the rare LVNC phenotypes is a combination with congenital heart defects, including atrial septal defect (ASD).
Brief description. The article presents a case report describing the difficulties of selecting antiarrhythmic therapy in a patient with LVNC and ASD, complicated by arrhythmias due to heart failure. The diagnosis of LVNC was confirmed by the Petersen criterion using magnetic resonance imaging.
Discussion. Cardiac arrhythmias in patients with LVNC and congenital heart defects, as a result of both anatomical and hemodynamic causes of electrical heart instability, constitute a danger of thromboembolism and sudden cardiac death, and also contribute to heart failure progression. The case is of interest due to the rare combination of LVNC and ASD, complicated by frequent episodes atrial fibrillation and premature ventricular contractions in the form of parasystoles, as well as difficulties in selecting antiarrhythmic therapy. Pulmonary vein cryoballoon ablation eliminated the source of atrial fibrillation. Ventricular ectopic activity was stopped using the anticonvulsant drug carbamazepine.
REVIEW ARTICLES
What is already known about the subject?
- Conservative treatment of migraine is recommended.
- Factors influencing the migraine course are in many ways similar to the clinical manifestations of a patent foramen ovale.
What might this study add?
- Foramen ovale closure relieves migraines.
- New clinical data show the effectiveness of foramen ovale closure in the treatment of migraine.
The literature review is devoted to the pathophysiology and clinical picture of migraine, targets of therapy and drugs used, and the connection between the pathogenesis of migraine with aura and patent foramen ovale is discussed. The results of clinical studies show a positive effect of endovascular patent foramen ovale closure on the course of migraine in the form of a decrease in the intensity, frequency of attacks and the number of headache-free days, as well as in some cases complete relief of the disease. Further study of the topic is promising, but requires careful study design and long-term follow-up of patients.
What is already known about the subject?
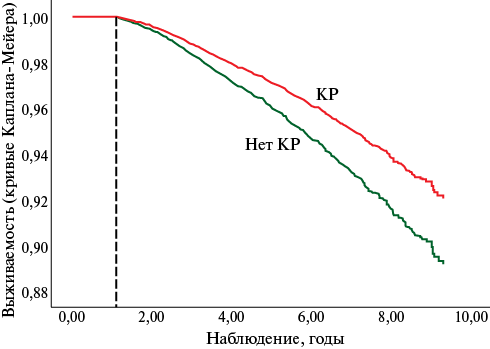
- Cardiac rehabilitation (CR) programs are an effective method for reducing the risk of cardiovascular events.
- Systematic physical training is a fundamental component of rehabilitation programs for cardiac patients.
What might this study add?
- Studies presented from different countries support the effects of exercise-based CR on reducing the risk of cardiovascular death, recurrent myocardial infarction, and hospitalizations.
- The reasons for the divergent influence of studies from different countries and meta-analyses examining the CR effectiveness on all-cause and cardiovascular mortality rates are analyzed.
The review discusses studies on clinical effects of exercise in patients after acute myocardial infarction and cardiovascular surgical interventions. Evidence of the high clinical effectiveness of training as an important component of cardiac rehabilitation programs is presented. The review presents the results of clinical studies on cardiac rehabilitation conducted in different countries.
What is already known about the subject?
- The problem of physician adherence to clinical guidelines and official drug labels is identified as a separate type of adherence, but has been studied much less well than patient medical adherence.
- To date, no classification of physician adherence/non-adherence to the implementation of the basic principles of rational treatment has been developed.
What might this study add?
- Using a literature search, the leading categories of physician adherence/non-adherence of doctors were identified.
- A classification of physician adherence/non-adherence to clinical guidelines and official drug labels has been developed.
The second publication is presented, devoted to the classification of the main parameters of quality and adherence to pharmacotherapy. Despite the fact that patients play a central role in the problem of medical adherence, the role of attending physicians is extremely significant both in prescribing/non-prescribing proven effective and safe therapy, and in influencing patient medical adherence. This led to the identification of a special commitment type — the physician adherence to the basic principles of rational treatment. Collection, analysis and systematization of information, as well as the related development of a classification of physician adherence/non-adherence were the aim of this review and analytical work. We searched data using keywords among Russian and English-language sources. When compiling the classification, categories of adherence/non-adherence were identified in accordance with the implementation by physicians of the main provisions of clinical guidelines for long-term therapy for patients with non-communicable diseases (NCDs), as well as following official drug labels reflecting data on clinical pharmacology, the main side effects, drug-drug interactions. The classification of physician adherence/non-adherence to implementing the principles of rational treatment of patients with NCDs can be used in the development of electronic medical decision support systems for providing therapy with proven effectiveness and safety in specific clinical situations. In addition, on the basis of the developed classification, checklists for monitoring by healthcare specialists of the implementation of the rational treatment of patients with chronic NCDs should be created.
ISSN 2619-0125 (Online)