ADDRESS TO THE READERS
RISK FACTORS FOR CARDIOVASCULAR DISEASES
What is already known about the subject?
- Existing SCORE and SCORE2 risk scales are widely used to assess cardiovascular risk, but have limitations in their application to the Russian population due to differences in epidemiology and risk factor profiles.
- The high prevalence of cardiovascular diseases and their risk factors in Russia requires accurate tools for risk stratification and optimization of preventive measures.
What might this study add?
- The developed PHOENIX score is a domestic tool for assessing the 10-year cardiovascular risk, adapted for the Russian population, differentiated for men and women.
- The PHOENIX score includes behavioral risk factors, psychosocial, and clinical parameters.
- The PHOENIX score offers a evidence-based, practical, and locally adapted method for cardiovascular risk stratification.
3Pavlov Ryazan State Medical University. Ryazan, Russia
Aim. To develop a national cardiovascular risk prediction score based on the prevalence of risk factors (RFs), their contribution to survival, and the occurrence of a composite endpoint.
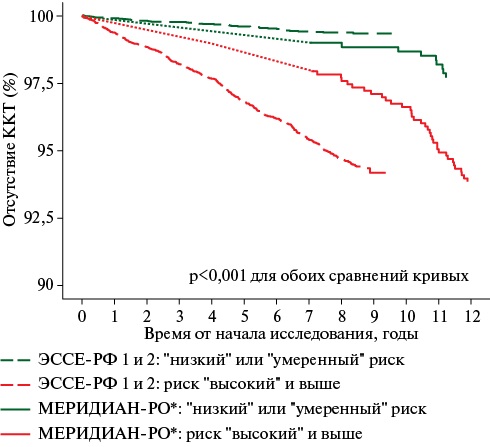
Material and methods. The prevalence of risk factors was studied in the cross-sectional studies ESSE-RF and ESSE-RF2. The prognostic value of risk factors was assessed during subsequent prospective follow-up. The algorithm was developed using a sample without prior myocardial infarction, stroke, or diabetes at baseline. Validation was performed using the MERIDIAN-RO study. Statistical analysis was performed in R (version 4.2). Kaplan-Meier curves and Cox models were used. Sex and region were included in the stratified model, while the remaining covariates were included in the regression equation. Multicollinearity was assessed using a variance inflation factor. The resulting relative risk scores were converted to an absolute 10-year probability of the composite endpoint using the Fine-Gray model. Validation was performed using the Cox model and C-indexes. Differences were considered significant at p<0,05.
Results. We excluded factors that were not modifiable by prevention and treatment, factors requiring special training for collection, biomarkers, and RFs without a significant association with the endpoint. The risk score for men included smoking, high blood pressure, tachycardia, hyperglycemia, poor self-rated health, adding extra salt to food, and a visual analog scale score <70. For women, we additionally excluded hyperuricemia, obesity, and high stress levels. The beta coefficients of the multivariate model were transformed into integers (0100). The 10-year probability of cardiovascular events was calculated in the following risk categories: "low", "moderate", "high", "very high", and "extremely high". External validation confirmed the scale prognostic significance (C-index 0,65).
Conclusion. Russian 10-year cardiovascular risk prognostic scale PHOENIX was developed as a tool for cardiovascular risk stratification in primary prevention.
What is already known about the subject?
- Current research demonstrates a significant impact of stress on the risk of adverse events, particularly cardiovascular events, among the adult population.
- The issue of stress in the context of healthy aging strategy is a relevant area for public health.
What might this study add?
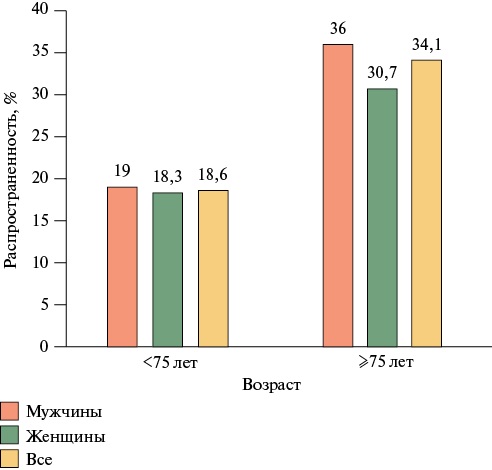
- Among middle-aged and elderly participants (<75 years), 18,6% experienced high levels of stress, while among elderly individuals (≥75 years), it was 34,1%.
- Among men over working age (≥63 years), the prevalence of high levels of stress was higher in those without higher education, with a low income, and prior myocardial infarction and cerebrovascular accident. Among women over working age (≥58 years), the prevalence of high stress was greater in those with a low income, a physical labor job, and a history of cerebrovascular accident.
- In a multivariate analysis among post-working age people, high stress levels were associated with an increase in all-cause death risk by 1,24 (p=0,049) among men and by 1,32 (p=0,02) among women, and with a 1,38-fold (p=0,049) increase in cardiovascular death risk among women.
Aim. To study the associations between high stress levels and the risk of all-cause and cardiovascular mortality in post-working age adults.
Material and methods. This representative sample of post-working age Moscow population (652 men aged ≥63 years, 920 women aged ≥58 years) from the Stress, Aging, and Health in Russia (SAHR) study. Stress was assessed using the Perceived Stress Scale-10 (PSS-10). High stress levels were defined at score of ≥21 for men and ≥24 for women, corresponding to the fifth quintile of stress levels. During the median follow-up period of 13 years, there were 832 and 442 all-cause and cardiovascular deaths, respectively. Statistical analysis was performed using STATA 14.0.
Results. In a multivariate analysis adjusted for sociodemographic and behavioral risk factors and noncommunicable diseases, high stress levels were associated with a 1,24-fold (p=0,049) increase in the risk of all-cause mortality among men and a 1,32-fold (p=0,02) increase among women. Regarding the risk of adverse cardiovascular outcomes, only women showed significant associations with high stress levels as follows: hazard ratio (HR) =1,38 (p=0,049).
Conclusion. A study among post-working age individuals revealed a significant impact of psychosocial factors, particularly stress, on the risk of all-cause mortality, which must be considered when developing preventive strategies for the elderly.
PUBLIC HEALTH, ORGANIZATION AND SOCIOLOGY OF HEALTHCARE, MEDICAL AND SOCIAL EXPERTISE
What is already known about the subject?
- Preventive counseling and remote monitoring of behavioral risk factors can promote sustainable weight loss and lifestyle modification in patients with noncommunicable diseases (NCDs), but their effectiveness in primary care requires further study.
What might this study add?
- For the first time in Russia, the comparable effectiveness of intensive preventive counseling followed by remote monitoring for patients with and without NCDs has been confirmed in real-world practice.
- Patients with NCDs have been found to demonstrate high adherence to remote monitoring, as evidenced by significant changes in the monitored parameters.
- The data obtained confirm the rationale of developing a management and functional model integrating intensive preventive counseling and remote monitoring into clinical follow-up through interdisciplinary collaboration between a local physician and a preventive health specialist.
Aim. To evaluate the effectiveness of digital technologies for intensive preventive counseling followed by remote monitoring of behavioral risk factors (BRF) for overweight in patients with noncommunicable diseases (NCDs) in a real-world practice to validate a management and functional model of interdisciplinary collaboration between a primary care physician and a preventive medicine specialist.
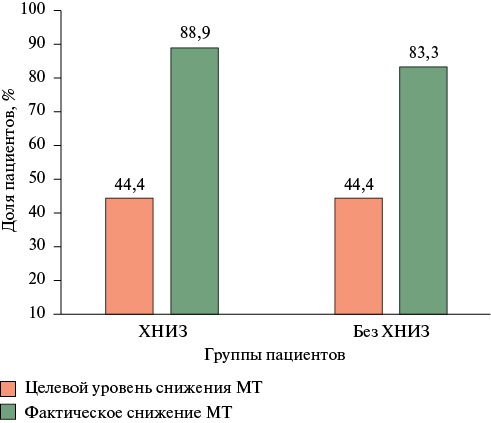
Material and methods. This prospective comparative cohort study was conducted among patients with a BMI ≥25 kg/m2 who underwent a clinical trial followed by remote monitoring of the PFR using the Doctor PM digital platform at healthcare facilities in three Russian regions. Of the 306 patients who completed the initial visit, 250 ended the 6-month follow-up period. A case-control study was conducted to form a study group of 72 patients with NCDs subject to outpatient follow-up and a control group of 72 patients without NCDs, stratified by age. Intensive preventive counseling was conducted with the setting of individualized goals for weight loss and BRF modification, including poor diet and low physical activity. Patients reported their weight, steps, and blood pressure (BP) data every 3 days for 6 months, and also completed a food frequency questionnaire in a mobile app once a week. Statistical analysis included intergroup (Mann-Whitney U-test, chi-square test) and intragroup (Wilcoxon signed-rank test) assessment at a significance level of p<0,05.
Results. Analysis of intergroup differences in dietary habit changes revealed significant differences in the consumption of vegetables, fruits, and grains (p=0,043). By the end of the follow-up period, it was higher in the group with NCDs. This group also showed a decrease in salt intake, while patients without NCDs more often reduced their intake of fats and simple carbohydrates. In the first month, physical activity levels were higher in patients without NCDs (p=0,019). From the second month until the end of the study period, no intergroup differences were observed (p>0,05). The decrease in body weight (BW), body mass index (BMI) and waist circumference (WC) was comparable in both groups as follows: BW -3,95 kg [-1,8; -7,6] (NCDs) and -4,0 kg [-1,0; -7,3] (without NCDs), p=0,34; BMI -1,3 kg/m2 [-0,7; -2,8] and -1,5 kg/m2 [-0,3; -2,8], p=0,35; WC -3,0 cm [0,0; -6,8] and -2,0 cm [0,0; -6,0], p=0,22 (intragroup p for all <0,001). The proportion of those who achieved BW reduction ≥5% was the same — 44,4% in each group (p=1,000). No intergroup differences were found in the frequency of BP data transmissions (p=0,906). Intragroup analysis showed reductions in SBP and DBP in the NCD group (p=0,025; p=0,019) and a reduction in DBP without significant change in SBP in the non-NCD group (p=0,005; p=0,065).
Conclusion. The obtained results indicate comparable effectiveness of organizational technology for intensive preventive counseling with remote monitoring of BRFs using the Doctor PM platform in both patients with NCDs eligible for outpatient monitoring and patients without NCDs. Positive changes in monitored indicators and high patient adherence suggest integration of this technology into outpatient follow-up through an organizational and functional model of interdisciplinary collaboration between general practitioners and preventive medicine specialists. The findings also provide grounds for extending the use of this technology to patients with behavioral risk factors, in particular those with overweight and obesity not eligible for outpatient follow-up, to foster sustained motivation for dietary behavior correction and regular selfmonitoring at earlier risk stages.
What is already known about the subject?
- Improving public health literacy is one of the fundamental components determining the effectiveness of preventive interventions.
- Women's health literacy is an important component enabling them to actively participate in health promotion activities.
What might this study add?
- Assessing women's health literacy helps identify their health information management skills and target groups for which educational programs and preventive measures should be developed and implemented first.
Aim. To assess health literacy (HL) among participants of the "Woman — a Health Model" project in the Republic of Buryatia.
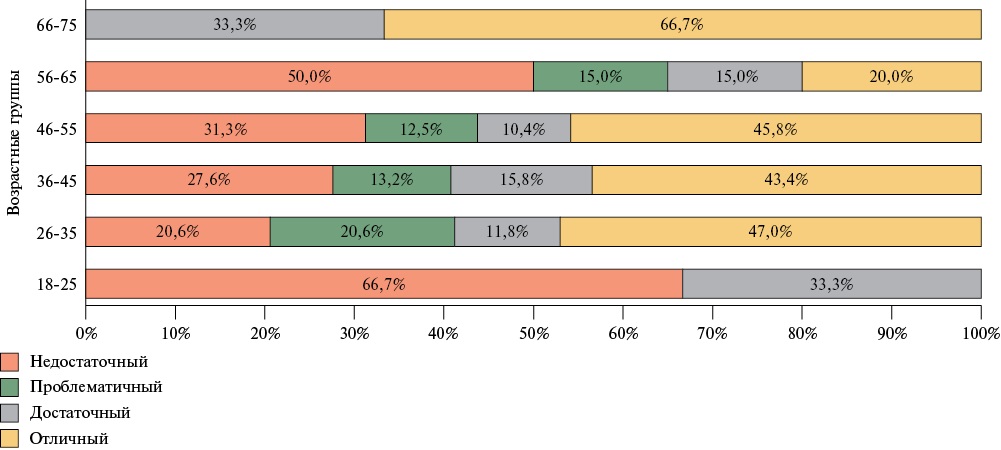
Material and methods. The "Woman — a Health Model" project was implemented in the Republic of Buryatia. A total of 184 females aged 18 and older were surveyed online to assess their health status using the validated HLS19-Q-RUS questionnaire, developed based on an international questionnaire and standardized indices for four levels of health status. The survey also included a preventive dictation.
Results. An assessment of the health status of project participants in the Republic of Buryatia revealed that 50% of women had insufficient and problematic health status. Women aged 18-25 (66,7%) experienced the greatest difficulties in managing health information. According to the preventive dictation, only 50% of respondents in the 46-55 and 66-75 age groups correctly defined the concept of "health". Moreover, in the 18-25 age group, the understanding of this term is 100% incorrect. Furthermore, respondents of this age group lack a proper understanding of certain basic principles of healthy eating.
Conclusion. A low and insufficient level of HL was identified among project participants in the Republic of Buryatia, which made it possible to identify key areas for training women in the fundamentals of a healthy lifestyle and health information management skills based on the data obtained.
CARDIOMYOPATHY
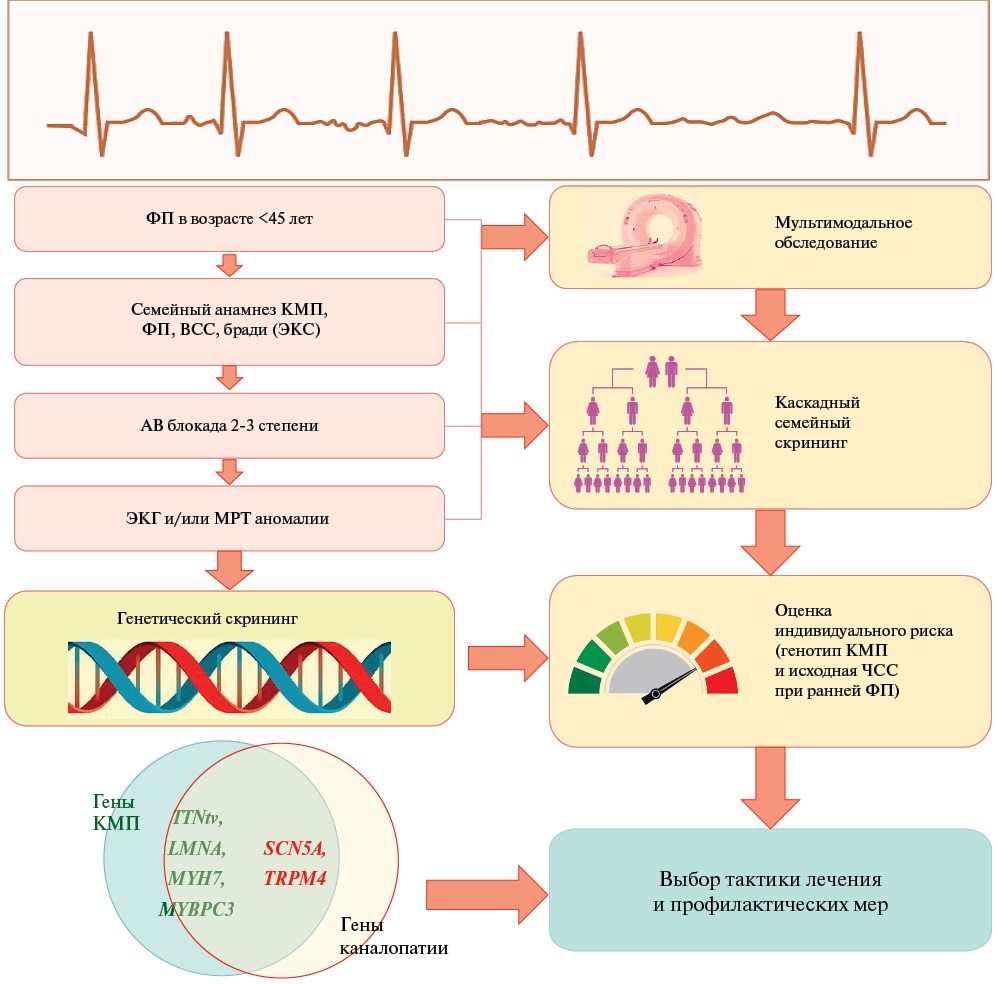
What is already known about the subject?
- Atrial fibrillation (AF) in cardiomyopathy is determined by multiple mechanisms associated with the genetic substrate, epigenomic, and population risk factors.
- The addition of AF to cardiomyopathy worsens the disease prognosis with an increased risk of death and hospitalization for stroke and heart failure.
What might this study add?
- A decrease in survival was demonstrated in patients with early AF, first recorded at age <45 years. Early development of AF in genotype-positive patients with cardiomyopathy (dilated cardiomyopathy/non-dilated cardiomyopathy) is associated with a 2-fold increased risk of cardiovascular death.
- Titin‐truncating variants (TTNtv), lamin A/C gene (LMNA) mutations, and pathogenic variants in the major sodium channel Na V1.5 gene (SCN5A) are associated with early-onset AF and cardiomyopathy.
- A cardiomyopathy genetic risk score has been developed for personalized risk stratification as an alternative tool for selecting patients with a high expected probability of a positive genotyping result.
Aim. To study the genotype and phenotype cardiomyopathy profile with atrial fibrillation (AF), as well as to evaluate the clinical outcomes and prognostic significance of genotyping early manifestations of AF in patients with dilated cardiomyopathy (DCM) and non-dilated left ventricular cardiomyopathy (NDLVC).
Material and methods. The study included 220 genotyped patients with cardiomyopathy as follows: 186 patients with DCM — 127 (68,3%) men, aged 44 [34; 55] years, left ventricular ejection fraction (LVEF) 30 [25; 36]%; 34 patients with NDLVC — 23 (67,6%) men, aged 35 [32; 41] years, LVEF 53 [47; 60]%. The follow-up period was 7 years with Me of 85 [69; 202] months. The cohorts were compared for the incidence of early-onset AF (at age <45 years), the genetic profile of cardiomyopathy, and clinical outcomes.
Results. Early-onset AF (paroxysmal, persistent, or permanent) was registered in 48 patients aged 35,3±6,8 years, while late-onset AF — in 33 individuals aged 53,2±3,7 years. Pathogenic variants in the LMNA, TTN, and SCN5A genes, identified in 19 (54,3%) patients, accounted for more than half of all genotypes with early-onset AF. In the laminopathy cohort (n=19), the prevalence of early-onset AF phenotype was the highest and amounted to 52,6%. Among all patients with early-onset AF, the prevalence of LMNA mutations was 20,8%; loss-of-function TTN variants were detected in 12,5%. The probability of detecting a cardiomyopathy-related variant was highest (odds ratio (OR) 17,4; 95% confidence interval (CI): 4,49-69,1) in individuals with early AF diagnosed at the age of <34 years with a family history of cardiomyopathy, and lowest in those >50 years old (χ2=30,2; p<0,001). Multivariate Cox regression analysis revealed that early AF with the pathogenic cardiomyopathy genotype was an independent predictor of cardiovascular death (hazard ratio (HR) 2,11; 95% CI: 1,09-4,07; p=0,027).
Conclusion. Variants in the LMNA, TTN, and SCN5A genes predominate in patients with genetic cardiomyopathy and early AF. Significant associations were found between genotype-positive cardiomyopathy with early-onset AF and unfavorable outcomes.
КАРДИОРЕАБИЛИТАЦИЯ
What is already known about the subject?
- Low total physical activity (TPA) is common in patients with heart failure (HF).
- Low TPA is associated with a higher all-cause and cardiovascular death risk.
What might this study add?
- More than a third of women and more than half of men with HF report low TPA. Those at highest risk for low TPA include women over 70 years of age, without a higher education, and with heart failure with preserved ejection fraction.
- The main factor limiting an increase in TPA is the bothersome symptoms during physical exertion.
- The next most significant factor is a lack of awareness about the physical activity benefits for HF treatment.
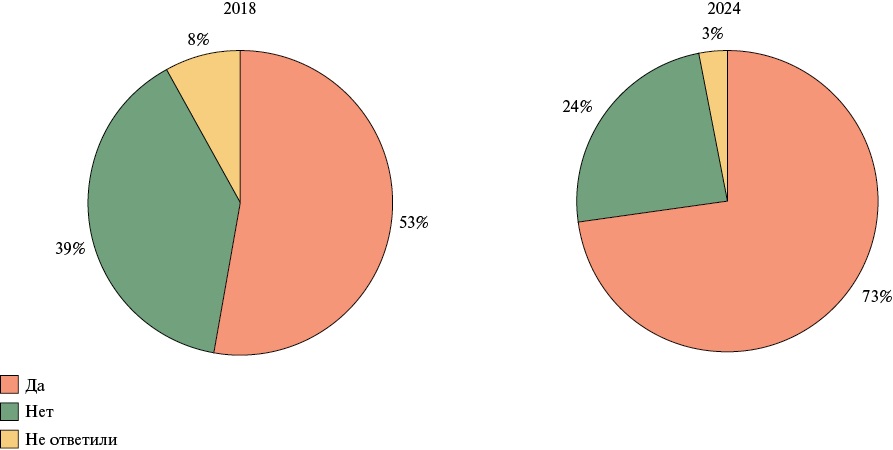
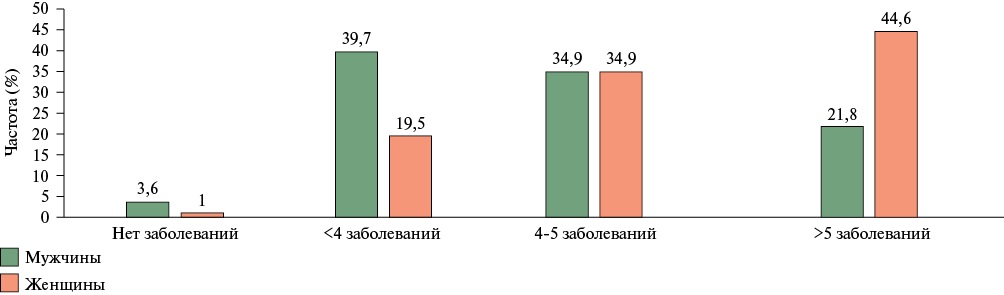
Aim. To analyze the sociodemographic, clinical, and behavioral characteristics of patients with heart failure (HF) based on their selfassessed current level of total physical activity (TPA), as well as changes of TPA and awareness of its benefits over time.
Material and methods. This cross-sectional survey was conducted in 2018 and 2024 as part of "HF Awareness Days". The self-administered questionnaire included questions about social status, TPA level, and attitudes toward physical activity as a treatment method for HF. Physicians completed brief information about the phenotype and functional class of HF.
Results. In the second wave of the survey, the number of unemployed patients who characterized their TPA as low or extremely low increased as follows: 74% of women and 64% of men in 2018 and 82% of women and 70% of men in 2024. Patients with a low TPA were more likely to report hospitalizations in the last six months preceding the survey. No higher education increased the odds of low TPA by more than 2,5 times in women (odds ratio (OR) =2,62; 95% confidence interval (CI): 1,360-5,126; p=0,003) and more than 3,5 times in men (OR=3,59; 95% CI: 2,06-6,26; p<0,001). Living with a spouse or children did not show a significant association with the TPA level. In women with HF, preserved ejection fraction (HFpEF) increased the likelihood of low TPA (OR=2,83; 95% CI: 153-5,34; p<0,001), while in men, HFpEF decreased the likelihood of low TPA (OR=0,425; 95% CI: 0,239-0,757; p<0,001). In addition, 67% of patients indicated bothersome symptoms as the reason for decreased activity. Women with low TPA were 3 times less likely, while men were 2 times less likely to consider exercise a method of HF treatment (OR=3,05; 95% CI: 1,64-5,67; p<0,001) and (OR=2,181; 95% CI: 1,422-3,362; p<0,001). In 2024, more patients acknowledged the exercise benefits than in 2018 (OR=2,3; 95% CI: 1,5-3,5; p=0,001).
Conclusion. More than a third of women and more than half of men in both waves of the study reported low total physical activity (TPA). Those at highest risk for low TPA include women over 70 years of age, without a higher education and with HF. Patients who described their lifestyle as inactive were significantly more likely to be unaware of the benefits of exercise for HF.
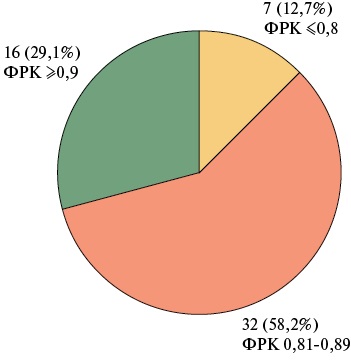
ENDOVASCULAR CORONARY INTERVENTIONS
What is already known about the subject?
- Optimizing the percutaneous coronary intervention (PCI) outcomes is one of the most pressing issues in modern endovascular practice.
- The conventional angiography-guided PCI does not always achieve the target outcomes.
- The use of coronary physiological indices is considered a promising solution.
What might this study add?
- Angiography-guided stenting fails to eliminate ischemia in one-third of cases, and in 50,9% of cases, it fails to achieve the optimal PCI outcome.
- The use of fractional flow reserve methods allows not only to assess the significance of coronary artery stenosis but also to improve PCI outcomes.
Aim. To assess the achievement of optimal outcome criteria based on fractional flow reserve (FFR) data during coronary physiology-guided percutaneous coronary intervention (PCI) with in patients with stable coronary artery disease (CAD).
Material and methods. A total of 150 patients with stable CAD and borderline coronary stenosis were initially recruited. After applying the exclusion criteria and FFR assessment, 55 patients were included in the study. They underwent angiography-guided stenting with FFR reassessment after the intervention. In residual ischemia, additional procedures were performed to optimize the outcome with intracoronary physiology reassessment.
Results. When evaluating outcomes using the physiological index, we found that stenting did not eliminate ischemia in 15 cases (27,3%), and optimal FFR values were achieved in only 12 (21,8%) patients. Optimization of PCI outcomes was required in 17 (30,9%) patients. After optimization, residual ischemia persisted in 7 (12,7%) patients, while optimal physiological index values were not achieved in 32 (58,2%) patients. Optimal FFR values were achieved in only 16 (29,1%) patients.
Conclusion. The use of intravascular physiology methods makes it possible not only to assess the significance of coronary artery stenosis but also to improve PCI outcomes.
STUDIES AND REGISTERS
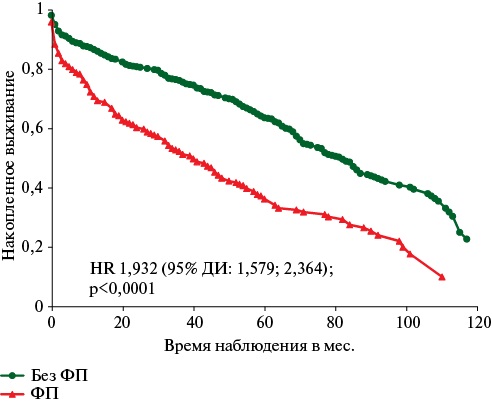
What is already known about the subject?
- Atrial fibrillation after stroke has a poor prognosis and is associated with an increased death risk.
What might this study add?
- Atrial fibrillation after stroke has a poor prognosis and is associated with an increased death risk at earlier stages of outpatient follow-up, but loses its independent prognostic significance later, giving way to other factors.
Aim. To study the prognostic value of atrial fibrillation (AF) during longterm follow-up of patients with cerebrovascular accident (CVA).
Material and methods. The study was conducted as part of the prospective part of the retrospective-prospective registry REGION-M registry. A total of 684 patients discharged from the hospital with a confirmed CVA between 2012 and 2017 and assigned to an outpatient clinic were included. The median follow-up was 5,0 [2,0; 6,8] years. AF was determined based on the diagnosis during the patient's hospital stay and/or at the first outpatient visit after discharge. The primary endpoint was all-cause death. An analysis of AF prognostic role was conducted for the entire follow-up period from hospital discharge to 2022.
Results. Patients with AF accounted for 29,2% (n=200). Comparison of the groups of patients with and without AF showed that patients with AF were older and had a higher number of comorbidities. AF had a paradoxical positive effect on the death risk (hazard ratio (HR) 0,998 (95% confidence interval (CI): 0,996-1,000), p=0,017). In this regard, we suggested that the AF effect on cumulative survival was disproportionate, i.e. changed over time. Therefore, the contribution of AF to death risk was assessed separately for three follow-up periods as follows: early outpatient follow-up — from discharge to contact in 20172018; intermediate — from the moment of the previous follow-up (2017 or 2018) to May 2020; long-tern — from 2020 to 2022. Differences in death risk between patients with and without AF were significant only in early (HR 1,003 (95% CI: 1,000-1,005) (p=0,016)) and intermediate (HR 1,004 (95% CI: 1,001-1,007) periods (p=0,016)). No significant differences in death risk between patients with and without AF were observed in the long-term follow-up period. Therefore, AF was not included in the multivariate regression analysis.
Conclusion. AF negatively impacts the death risk during the first 3-4 years after CVA. After this period, AF loses its independent prognostic significance.
What is already known about the subject?
- Studies show an annual increase in the incidence of pulmonary embolism (PE) with increasing life expectancy.
- Results from the global GARFIELD-VTE registry, published in 2023, showed a high mortality in patients with PE within 36 months of hospital discharge due to recurrent venous thromboembolism (VTE).
- The most common cause of death was recurrent PE following discontinuation of anticoagulant therapy.
What might this study add?
- Long-term 60-month follow-up of patients with PE identified a high-risk period for fatal recurrent PE — the first 12 months, during which secondary VTE prophylaxis with anticoagulant therapy should not be interrupted.
- The most common cause of death after the first year of follow-up was malignancy, along with recurrent PE.
- Prolonged anticoagulant therapy is received by ~30% of patients after PE, and during the 12-60 month follow-up period, deaths due to coronavirus disease 2019 and other cardiovascular diseases were more common.
- During the five-year follow-up period, a high incidence of non-severe bleeding (7,4%) was observed, with a single bleeding episode being the most common.
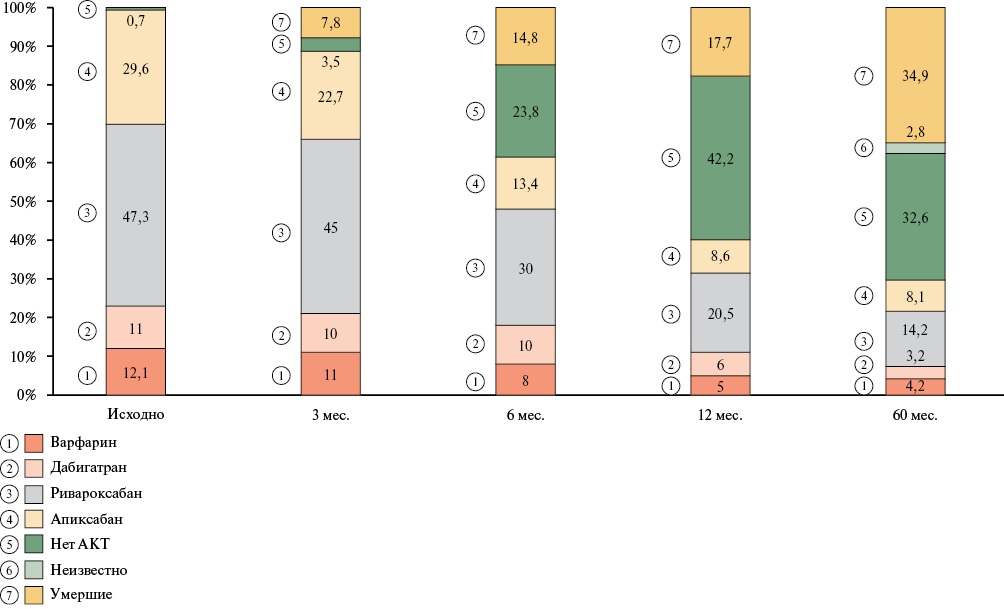
Aim. To evaluate the results of a five-year follow-up of patients included in the Russian Registry of Acute Pulmonary Embolism (SIRENA), available to the contact at this stage of monitoring.
Material and methods. The SIRENA registry is a prospective, multicenter, observational cohort study designed to evaluate the treatment outcomes of patients with pulmonary embolism (PE) In Russian hospitals. The primary endpoints were all-cause death, recurrent PE, and major bleeding. Bleeding severity was defined according to the BARC (Bleeding Academic Research Consortium) criteria.
Results. A total of 283 patients aged 32 to 97 years (mean age 69 (59-76) years) were enrolled at nine centers; 135 of them were men (47,0%). Over 5 years of follow-up, 99 of 283 (34,9%) patients died. The most common causes of death were cancer (14,1%), death related to coronavirus disease 2019 (COVID-19) (17,2%), and recurrent PE (16,2%). During the first year of follow-up, cancer and recurrent PE were most frequent mortality causes, while deaths from COVID-19 and other cardiovascular diseases were more common during the 12-60-month follow-up period. Long-term anticoagulant therapy was continued by 29,7% of patients with PE at 60 months of follow-up, with 21 patients (7,4%) having bleeding episodes during this period. Most commonly, patients experienced one episode of BARC type 1 bleeding, but three patients experienced 10 or more bleeding episodes, which were considered minor.
Conclusion. Thus, this five-year study of patients with PE provides an assessment of their treatment outcomes 60 months after PE and may form the basis for future research on venous thromboembolism. High mortality rates, recurrent venous thromboembolism, and bleeding events within five years of follow-up after diagnosis of PE highlight the importance of effective treatment and accurate risk stratification for adverse outcomes.
What is already known about the subject?
- Cardiovascular pathology remains the leading cause of death among the elderly population living in metropolitan areas, despite increased life expectancy due to a reduction in cardiovascular and cancer mortality.
- These results indicate the need to develop and update comprehensive programs for the clinical examination and preventive counseling of elderly patients.
What might this study add?
- Over the past 15 years, life expectancy in the metropolitan areas has increased by 7,4 years for men and 5,1 years for women.
- A reduction in cardiovascular and cancer mortality had a positive effect on the increase in average life expectancy.
- According to the population study, along with cardiovascular diseases, mental disorders, particularly cognitive impairment and depression, also contributed to all-cause mortality.
Aim. To assess the impact of cardiovascular disease (CVD) and other causes of death on life expectancy among elderly Muscovites over the past 15 years using population and demographic studies.
Material and methods. An analysis of the population-based study "Stress, Aging, and Health" (survey in 2007-2009; endpoints’ collection in 2024) and official statistics (2009 and 2023) was conducted. Statistical analysis was performed using STATA 14.0 and Excel 2024.
Results. According to the population-based study, CVD increased the risk of all-cause mortality by 1,87 times in men and 1,47 times in women. A similar effect was observed for mental disorders (hazardratios (HR) =1,49 and 1,24 for men and women, respectively). According to the demographic study, average life expectancy (ALE) in Moscow increased by 7,4 years for men and 5,1 years for women from 2009 to 2023. The main contribution to the increase in ALE was made by a decrease in mortality from CVD and cancer. Mental disorders also contributed to an increase in life expectancy by 0,139 years, predominantly in women.
Conclusion. Although CVD remains the leading cause of death in the elderly, current treatment and preventive measures demonstrate effectiveness. At the same time, the data obtained highlight the need to develop measures for the early detection and treatment of diseases specific to older adults, such as cognitive impairment and geriatric depression.
REVIEWS
What is already known about the subject?
- The composition of the Mediterranean diet was studied.
- The mechanism of action of several components of the Mediterranean diet was discovered.
- The benefits of this diet for vascular health were demonstrated, and the anti-atherosclerotic and anti-inflammatory properties of the Mediterranean diet were established.
What might this study add?
- Current information on the mechanisms of action and clinical efficacy of the main biologically active agents of the Mediterranean diet is presented and structured.
- The role of alcohol in the Mediterranean diet is discussed, and the results of clinical studies are critically analyzed.
- Promising approaches for cardioprotective diet standards are highlighted.
Among the proven risk factors influencing cardiovascular mortality, unhealthy diet plays a significant role. Currently, the most studied dietary pattern for its cardioprotective properties is the Mediterranean diet.
The aim of this review is to present current data on the key biologically active agents of the Mediterranean diet, their mechanisms of action, and the evidence base for their clinical efficacy in the context of cardiovascular prevention. The review for each active agent is structured into subsections, including: a) a list of plant-based foods containing the active agent; b) a summary of the agent's mechanisms of action; and c) the evidence base for its clinical efficacy.
The authors hope that the information presented in this review will be useful to primary care physicians, internists, and cardiologists and can be applied in their practice to prevent cardiovascular diseases and improve patients' quality of life.
What is already known about the subject?
- The idea of a tobacco endgame is based on tobacco control recognition as the first priority for the prevention of noncommunicable diseases.
- The concept of a tobacco endgame implies a transition to the implementation of policies and strategies aimed at the complete elimination of tobacco use.
What might this study add?
- Policy initiatives, strategies, and measures of a tobacco endgame, as well as country experiences in implementing them, are systematized.
- To achieve tobacco control goals, regulations need to be revised to include product- and consumer-focused measures.
- Comprehensive measures combining several strategies aimed at ending the tobacco epidemic appear to be the most effective.
More and more countries are implementing strategies aimed at ending the tobacco epidemic. The aim of this three-article study was to analyze existing tobacco endgame strategies and measures, their potential or actual effectiveness, assess the implementation of these strategies within national legislation, identify the main barriers to their implementation, and discuss prospects for achieving them. This article systematizes tobacco endgame policy initiatives, strategies, and measures, as well as analyzes productand consumer-focused policy initiatives, the strategies and measures implemented within these initiatives, and their effectiveness.
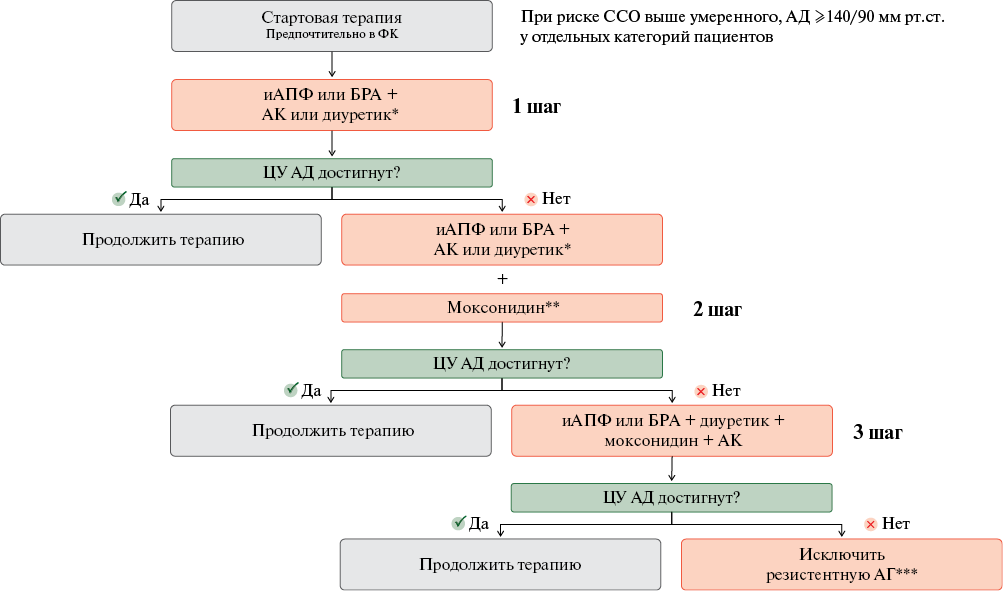
EXPERT CONSENSUS
What is already known about the subject?
- The growing number of patients with multimorbidity and complex pathogenesis of hypertension (HTN) requires a personalized approach to treatment taking into account the etiology, clinical phenotype, and comorbidities.
What might this study add?
- The authors' consensus on personalized therapy for HTN in patients with comorbidities is substantiated. A new term, "acute blood pressure increase without target organ damage" or "uncontrolled hypertension," is proposed.
- Early initiation of combination therapy using an imidazoline receptor agonist (moxonidine), which improves a wide range of HTN-related pathologies, makes an important contribution to cardiovascular risk reduction.
Hypertension (HTN) is a serious public health problem. Despite advances in diagnosis and public awareness, the percentage of controlled cases remains low, especially among men and the elderly. The main challenges are related to comorbidities such as obesity, diabetes, chronic kidney disease, and obstructive sleep apnea, which worsen the prognosis and increase the risk of cardiovascular events.
The approach to HTN treatment should be individualized and take into account specific disease phenotypes and comorbidities. It is important to identify patients with increased sympathetic nervous system activity, as this group experiences the greatest difficulties in blood pressure control. Moxonidine, a centrally acting agent, selectively stimulates imidazoline receptors in the brain, causing a decrease in sympathetic activity and effective reduction in blood pressure.
The need for a personalized approach to HTN therapy is driven by the growing number of patients with multiple comorbidities and complex pathogenesis. New approaches, including early initiation of combination therapy and targeted management of metabolic risk factors, will reduce cardiovascular morbidity and mortality. Moxonidine plays a key role within antihypertensive medications due to its unique mechanism of action and ability to positively impact a wide range of HTN-related pathologies
ISSN 2619-0125 (Online)